Sepsis
An infection that spreads through the body is sepsis. An individual can develop an infection anywhere in their body, which most often will stay in that body part. Occasionally, the infection can spread to other parts of your body including major organs. Sepsis develops quickly. Your body is unable to control the infection which can lead to organ failure, tissue damage, and death. Sepsis is a serious, life-threatening situation.
Infections can begin from a pathogen which includes bacteria, viruses, fungus, or parasites, entering the body. A rare source of infection is prions which occurs when harmless proteins in the brain change creating neurodegenerative diseases such as Creutzfeldt-Jacob disease, and spongiform encephalopathies among others. Bacterial infections are the most frequent causes of sepsis. The most common viral causes include influenza (flu) and COVID-19. However, any pathogen in the body can lead to sepsis.
When one or more pathogens enter the body and multiply, infections begin. Typically, when the invader is recognized by your body, the immune system sends white blood cells and naturally occurring antibodies to eliminate the pathogen. Results of the immune system working may include symptoms such as fever, headache, rash, and tiredness, all of which help the body fight the invader.
In some cases, the pathogen overwhelms the immune response. The pathogen continues to multiply which enables it to enter your circulation. Blood then carries the pathogen throughout the body which triggers an inflammatory response. As the pathogen is in your circulation, it can enter major organs of your body and body tissue where it continues uncontrolled multiplication of cells leading to damaging and overpowering normal body functions. This is sepsis.
Sepsis can affect the body to the point of creating a severe drop in blood pressure. When this occurs, septic shock is diagnosed. This is an extremely critical time as cells in the body are affected, making them less able to function and produce energy for the body. Sepsis can lead to death, but the risk of death is significantly increased in septic shock.
Individuals with neurological diseases or injuries may have an increased risk of sepsis due to the effects on the autonomic nervous system (ANS). The autonomic nervous system controls body functions that occur automatically without your conscious control. Much like the automatic beating of your heart, the ANS also influences the response of the immune system. If the ANS is affected by neurological disease or injury, it may be slow in response to trigger the immune system to react, may not respond effectively to control the invader, or may not react to the presence of an invader at all. This allows the pathogen to multiply uncontrolled.
The outcome of sepsis is wide-ranging. Some individuals survive without any consequences or deficits. Others may have a temporary or permanent injury to one or more internal organs such as brain injury, cardiac failure, breathing difficulty, or loss of limb or other body parts. Blood clots and ruptures in large and small blood vessels lead to damage throughout the body. The outcome for some individuals is death.
If you think someone has sepsis, call 911. If in the hospital, bring the symptoms to the attention of the physician or registered nurse. Sepsis is a medical emergency. Fast care can save a life.
How Infection Begins and Treatment
Pathogens can enter the body through mucous membranes consisting of the eyes, nose, mouth, urogenital openings, or rectum, or through skin wounds and sores including pressure injuries and bites. Some bacteria live naturally in the body to help function such as certain bacteria in the bowel that help digest food. However, these bacteria can proliferate overwhelming your normal body system. Ways pathogens enter the body are:
Contact – touching a contaminated surface and then rubbing your eyes, mouth, nose, urethra, vagina, or rectum. Contact transmission includes pathogen entry through any mucous membranes, body fluids, and infected skin.
Vehicles – include pathogens entering the body through substances such as contaminated water, food, or infected blood.
Vectors – comprise contaminates introduced to an individual by other creatures, most commonly the mosquito, but also fleas, ticks, mites, rats, snails, and dogs.
Airborne – include evaporated droplets and dust particles that are inhaled into the body.
Early identification and treatment of infection are critical to avoid the infection evolving into sepsis. Take measures to stop infections before they begin.
Check to ensure your water is safe. Water companies manage water contamination and will alert you if your water source is contaminated. Boil orders will be in place for you to boil your water if it is necessary. Individuals using well water will need to have their water regularly tested to ensure safety.
Wash your hands frequently with soap and warm water or if that is not available, use hand sanitizer. Cleanse your hands after toileting (before and after catheterization and bowel programs) and when handling any dirty item.
Wear a mask and social distance if you are unsure about your surroundings or if you are immunocompromised. Following the rules of COVID-19 will help reduce your exposure to other pathogens.
Cook food to appropriate temperatures to ensure safety. Wash your hands before and after handling food, especially raw food. Carefully clean dishes and cooking supplies. Keep foods refrigerated as needed.
Clean your body daily with soap and warm water. Use clean washcloths and towels to avoid bacteria recontamination. If your body becomes soiled, wash and dry immediately and wear clean clothes. If your skin becomes open from a cut, scrape, or bite, wash immediately with soap and water, covering with a sterile bandage. Large wounds should be evaluated by a healthcare professional for treatment.
Cover your mouth when coughing or sneezing, using a tissue followed by immediately placing it in a trash receptacle. Then wash your hands. Request/insist others around you do the same. Wear a mask if you are in an area with high contamination or respiratory transmitted illnesses.
Keep your hands away from your eyes, nose, and mouth as well as your urethra, vagina, and rectum. These moist, mucous membranes are where pathogens like to invade the body.
If you use communal equipment, such as gym equipment or public transportation, clean the area before and after contact and wash your hands.
If you develop an infection, seek treatment from your healthcare provider immediately as stopping an infection from spreading is necessary to avoid sepsis. Take antibiotics only as specified by your health professional who will provide testing to make sure you receive the correct medication. Take the medication for the full dose even if you feel better. This will eradicate the pathogen.
Think about your activities in regard to pathogens and what you can do to ensure your safety. Pathogens are all around us, usually causing no harm. However, be mindful about what you are doing and where you are going to maintain your health.
Risks for Sepsis
Anyone can get sepsis at any time. This includes fetuses in utero, infants, children, adults, and seniors. No one is exempt from the risk of sepsis. Some individuals who use improperly cleaned gym equipment suddenly develop sepsis or those without health issues develop it without clarity of cause.
However, some individuals are at a higher risk. These include babies under one year of age, adults 65 years and older, individuals with chronic health conditions such as diabetes, cancer, lung, liver, and kidney disease, those with weakened immune systems, those taking immunosuppressant medication or have neurological effects of the autonomic nervous system (ANS), those with current infections or severe illness or those who are hospitalized especially for long periods of time.
Individuals in the intensive care unit (ICU) are at an increased risk, not because of their location in the hospital but because they are critically ill. Artificial openings in the skin from catheters, intravenous fluids (IVs), or ventilatory tubes can be an entry point for infections leading to sepsis. Medications such as antibiotics, especially with overuse or overtreatment, and corticosteroids can increase the risk of sepsis as both can lower the immune system response. Individuals who have had sepsis are at a higher risk of reoccurrence of sepsis and of increased numbers of respiratory infections.
Signs of Sepsis
Signs of sepsis may occur slowly or quickly. Many individuals who develop sepsis are typically already hospitalized for something else, but individuals living in the community, especially those with neurological issues can develop sepsis. Therefore, the individual, family, and caregivers must know the early signs of sepsis. The individual may not be able to recognize the signs themselves due to mental changes from sepsis or changes in body function due to sensation issues. Always ask, ‘could this be sepsis’ to any healthcare provider to promote early treatment.
Signs of sepsis may include some or all of the following. Not everyone may have every sign. Individuals with neurological disease or injury may have muted signs due to effects of the autonomic nervous system and sensation issues.
- High heart rate (pulse) or higher than your individual normal heart rate
- Low blood pressure or lower than your individual normal blood pressure
- Fever, shivering, or cold feeling, clammy or sweaty skin, these symptoms may appear only above your level of injury in SCI or on one side of the body with hemiplegia
- Confusion or disorientation (may be more sudden or profound in individuals with brain injury, the elderly, or those with dementia)
- Shortness of breath
- Severe pain or discomfort, if body sensation is an issue this may feel more like a sensation of anxiety, feeling that ‘something is not right,’ or impending doom
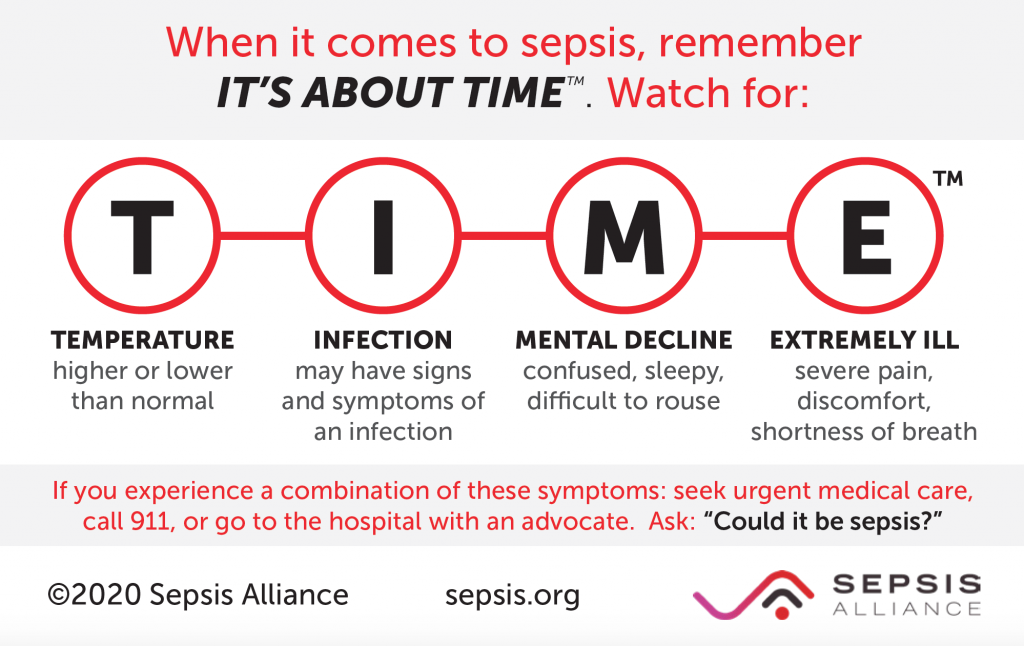
This card below, created by the Sepsis Alliance, helps assist with monitoring the warning signs of sepsis. Be sure you have the card. Provide it to caregivers, teachers, and other individuals as appropriate.
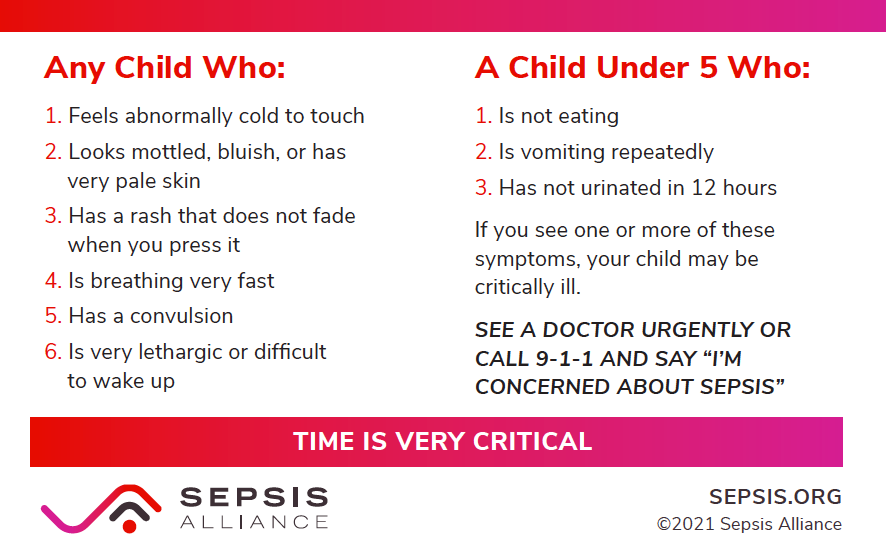
Because of differing developmental and communication issues, children may be ill but not express their feelings to an adult. This card below from the Sepsis Alliance indicates sepsis symptoms in a child:
Symptoms of Sepsis
Sepsis may develop after an infection. Not all infections lead to sepsis. Knowing you have or recently had an infection, even if treated, should put you on alert for sepsis. However, for some individuals, sepsis seemingly appears out of nowhere. It may be that an infection was present without your knowledge or that the symptoms of infection were not felt due to sensory issues or that the infection was confused for a separate medical issue.
Symptoms of sepsis include:
- Infection presence whether known or unknown.
- Mental status changes such as lethargy, sleepiness, hard to waken, fogginess, confusion, disorientation, agitation, and any change in behavior or interest. Elderly individuals or those with dementia may develop a sudden change in mental status or an increase in dementia symptoms.
- Blood pressure changes with the systolic blood pressure (top number) below 100 mm Hg. This may be lower for individuals who have low blood pressure as their normal from spinal cord injury or other neurological issues.
- Breathing or respiratory rate of 22 breaths per minute or more. This might also be not noticed in individuals with neurological effects of reduced breathing function or those who require mechanical ventilation.
Symptoms of septic shock include:
- Medication is required to maintain systolic blood pressure (top number) greater or equal to 65 mm Hg.
- Blood tests result in high levels of lactic acid which indicates that body cells are not functioning so oxygen cannot be metabolized.
A helpful sepsis wallet card is provided by the Christopher & Dana Reeve Foundation for free. It is a quick guide of symptoms, treatments, and information for your healthcare provider. You can present this to a healthcare provider in an emergency or any situation to help stimulate early treatment.
The good news is, if you know the signs, and are quick to contact your physician when they set in, sepsis is treatable.
In order to help you be as aware as possible about sepsis, and to help your doctor to understand your susceptibility to the condition, the Reeve Foundation National Paralysis Resource Center (NPRC) offers a convenient and life-saving wallet card to draw immediate attention to sepsis.
Thanks to the collaboration of Linda Schultz, PhD, assistant professor of nursing at Maryville University, and the medical staff at Kennedy Krieger Institute, the sepsis wallet card was designed for both the patient and the physician, and applies to both adults and children.
Easy to fit in your wallet, the card is a tri-fold that will allow you to record your level of injury and include emergency numbers, review symptoms of sepsis, among other important information.
One of the folds is written specifically for the physician. In the event of a sepsis crisis, you can pull the “Attention Physician” flap to the front. This allows first responders to see your personal information on one side, and directions to treat sepsis on the other.
Copies of the sepsis wallet cards are available online for download, or you can get your laminated copy by calling the NPRC at 800-539-7309 and asking to speak to our Information Specialists.
The information contained in this card and web page is presented for the purpose of informing you about paralysis and its effects. Nothing contained herein is to be construed or intended as a medical diagnosis or treatment. Contact your physician or other qualified healthcare provider should you have questions on your health, treatment, or diagnosis.
The following video is a concise summary of sepsis:
Sepsis Notification Alert
If you think your family member may have sepsis, always mention ‘do you think this could be sepsis’ to emergency personnel if 911 is called, the emergency room physicians and nurses, or if in the hospital on a general floor or even the intensive care unit (ICU) to the physicians and nurses caring for the patient. Put sepsis forward in their mind. Many other more common issues and symptoms can be mistaken with sepsis as an overall diagnosis. Keep asking ‘could this be sepsis’ to get people thinking about it, so they will perform sepsis testing quickly and provide treatment early. The faster treatment begins, the quicker recovery can occur.
Avoiding Sepsis
Steps can be taken to help avoid sepsis. Along with the steps to preventing infection listed above, these additional steps will not make you immune to sepsis but will help you reduce your chances of spreading infection in your body.
- Wash your hands for 20 seconds (sing Happy Birthday twice) with soap and water frequently. Wash before and after handling food, after taking out the trash, after sneezing, before and after catheterization, bowel program, suctioning, or dressing changes, after toileting, or any other ‘dirty’ type of activity. Wash your hands when entering your home or just because you feel you should.
- Keep your body clean. Use clean towels after bathing.
- Properly dispose of used tissues immediately.
- If you have signs or symptoms of an infection, call your healthcare provider for an infection assessment.
- Take the full prescription of an antibiotic, antiviral, antifungal, or antiparasitic drug. You may feel better, but the pathogen is not out of your body until the entire medication is taken.
- Request the lowest generation of drugs that will treat your pathogen. Broad-spectrum medications can lead to resistance and other health issues.
- Be sure your vaccinations are up to date.
- Speak up if healthcare providers or caregivers do not wash their hands.
- Follow the suggestions from above to avoid an infection.
Diagnosing Sepsis
Diagnosis of sepsis can be challenging as it can mimic the symptoms of other healthcare issues. Several tests may need to be performed to get to a sepsis diagnosis. This is why is it so important to keep asking if the issue ‘could be sepsis’. The healthcare professional will first be thinking of sepsis based on the individual’s medical history including recent infection. However, some individuals may not know they had a recent infection, so testing is imperative.
Blood tests are performed aimed at two purposes. One is to look for infection or reactions to infection in the blood. This is done through the use of blood tests and blood cultures to quickly identify the presence and type of infection. The results indicating an infection is in the body will be evidenced by the presence of a pathogen and/or increased cells to fight infection. Another test is lactate measurement in the blood which indicates if there is sufficient oxygenation in the cells of the body. Other blood tests may indicate evidence of health issues such as poor clotting time, an inability to oxygenate the body properly, imbalances in the body’s electrolytes, and liver and kidney function which can indicate damage to these organs.
Specimen collection may include drainage from a wound, vomit, urine, stool, and respiratory secretions. These samples may contain pathogens that will indicate the presence of infection in the body.
Imaging studies are examinations of the internal body. Image studies that may be considered are X-rays and ultrasounds to look for infection, especially in the lungs or pockets of infection anywhere in the body. Computerized tomography (CT scan) or magnetic resonance imaging (MRI) are more specific imaging tests.
Assessment scales have been developed to evaluate organ systems affected by sepsis by healthcare professionals in a medical setting. These should not be used at home as the emphasis is to get the individual to a healthcare setting quickly.
The Sequential Organ Failure Assessment (SOFA) is used to assess the neurological, blood, liver, kidney, and hemodynamics (blood pressure) of the body. Some healthcare professionals will use this technical assessment.
A quick Sequential Organ Failure Assessment (qSOFA) was designed with three criteria. The criteria are low blood pressure, altered mentation (by use of the Glasgow Coma Scale), and respiratory rate.
Treatment of Sepsis
Sepsis is a medical emergency. It can move quickly through the body. If found early, less treatment will be needed and less damage to the body will occur. The further sepsis progresses, the more treatments will be required. Sepsis affects various parts of the body depending on the location of the infection, where it has spread, and the body parts affected.
Medications are required to treat the infection as well as to support body functions. The most typical medications are listed below. Additional medications and treatments are used as needed for each individual case.
- Antibiotics, antivirals, antifungals, or antiparasitic medication will first be ordered. If the source of the infection is known, the antibiotic, antiviral, antifungal, or antiparasitic that will destroy the pathogen is used. However, until testing can be performed to identify the precise pharmacological treatment, broad-spectrum antibiotics or other broad-spectrum medications will be used. Broad-spectrum medications can eradicate a variety of pathogens. This must be done to control the infection quickly. However, long-term use of broad-spectrum medications can lead to antibiotic resistance. Once laboratory tests for medication specifically for the individual’s infection are identified, that medication will be used. The use of broad-spectrum antibiotics affects the natural flora in the bowel which can lead to severe diarrhea caused by the bacteria Clostridium difficile (C diff). This further complicates sepsis treatment. Because of the emergent treatment needs for sepsis, the benefits of starting treatment with broad-spectrum antibiotics outweigh the risks of antibiotic overuse.
- Fluid resuscitation by IV will be supplied to keep the individual hydrated, increase fluid in the vascular system and tissues, and help reduce lactate in the body. Fluid is provided in four stages: Rescue, Optimization, Stabilization, and De-escalation.
- Blood pressure maintenance is provided by medications including vasopressors which constrict blood vessels to increase blood pressure. These help to increase blood flow to your major organs. If your blood pressure falls too low for your individual normal, these medications will be used.
Surgery may be required in the acute phase of sepsis to drain and clean an area of infection within the body. If a body part has not received oxygen and nutrients, dead tissue may need to be surgically removed.
Sepsis Bundles are evidence-based treatment plans for urgent care of sepsis. These are formatted plans that occur on a time schedule to provide quick and appropriate care needed for the treatment of sepsis. Included are screening for early identification of sepsis, guidelines for treatment, education for healthcare providers, and the use of best practices. Most healthcare facilities have a sepsis bundle protocol that is followed to improve the care of an individual with sepsis.
Other Treatments are provided depending on individual needs. For example, if blood glucose (sugar) is elevated (due to trauma) insulin may be needed, if breathing is affected mechanical ventilation will be used, kidney failure may be treated with dialysis, or cardiac failure may be treated with medications.
Post-Sepsis Syndrome
Recovery from sepsis can be an ongoing process. The effects of sepsis are challenging in many ways including mental well-being and physical changes. Some individuals have no changes in their physical abilities but may have mental health issues due to the trauma of severe illness. Others may also have physical challenges. Some have both mental and physical issues. Any concerns should be reported to your healthcare professional to ensure helpful treatment is provided.
Symptoms of Post-Sepsis Syndrome (PSS) may include some or all of the following:
Physical issues can be due to deconditioning of the body, difficulty with stamina, moving joints, changes in function due to amputation, or changes in organ function. There can be hair loss and rashes on the skin.
Mental issues can be due to the trauma of the illness and treatments. This can include near-death experiences, sleeping issues, nightmares, panic attacks, and post-traumatic stress disorder (PTSD). There may be temporary or long-standing issues in thinking, concentration, mood, and memory issues, depression, mood swings, and poor appetite.
Families may have changes in roles and dynamics. Independent individuals may become dependent after sepsis and require physical care as well as mental assistance. Transitioning to the home setting can be disruptive for the individual if they cannot resume previous responsibilities or are unable to recognize their deficits. This can be frightening for both the individual and the family. Counseling and mental wellness therapy are critical to learning the tools to deal with this situation for both adults and children.
Ongoing physical and mental healthcare is necessary for treatment and adjustment to new ways of doing activities of daily living and psychological issues. Individuals who have had sepsis are more prone to a second bout as well as respiratory infections.
The Rehabilitation Healthcare Team
During the emergency and acute phases of sepsis, you will be cared for by emergency medical technicians (EMTs), emergency room and intensive care personnel. Specialists will be required to provide treatment for body functions affected by sepsis. These may include specialists in the nervous system (neurologists), heart and vascular system (cardiologists), respiratory system (pulmonologists), liver function (hepatologists), kidney function (nephrologists), and blood dyscrasia issues (hematologists) among others.
When transitioning to the recovery phase of sepsis, the following specialists will assist with your recovery:
Physiatrists are physicians who specialize in physical and rehabilitation medicine. You may meet this individual during the acute phase of your illness or during rehabilitation. They will continue your care until your issues have been resolved. This individual will provide overall care and direction for your health needs. They will collaborate with your team of specialty providers to coordinate your care for the best outcomes.
Rehabilitation Nurses are individuals who will assist with integrating rehabilitation care techniques into self-care and work with caregivers who will provide care at home. They have expertise in many areas of care including bowel, bladder, and skin care in addition to coordinating your specialty services into your daily routine as you are able. A registered nurse will assist with the coordination of home care.
Respiratory Therapists are professionals that will assist with breathing strategies and respiratory comfort. They monitor your breathing ability, provide treatments, assist with keeping your airway clear, provide breathing exercises as well as mechanical ventilation if needed.
Physical Therapists provide advancing therapy for gross movement such as transferring, standing, and walking. They will progress your care as your strength and stamina improve, providing exercise to enhance your condition and equipment to increase mobility.
Occupational Therapists provide advancing care in finer movements such as hand and finger function. They provide care and education in activities of daily living (ADLs) such as bathing, dressing, toileting, and other functional actions. They will recommend equipment to increase your function.
Speech and Language Pathologists assist with swallowing and language as needed. They may use technology for communication until you are able to do so on your own. They are also adept at identification and stimulation of cognitive function.
Psychologists and/or Psychiatrists assist with mental wellness and strategies to cope with health issues and life changes following sepsis. They will provide care for both you and your family.
Psychometricians are individuals who can provide testing if needed to establish if there is injury within the brain that may affect function and mentation. They will present treatment strategies that your rehabilitation team can integrate into your care plan.
Wound Care Specialists are generally registered nurses or physical therapists who have specific education in the care of wounds. They will provide treatments for complex wounds that require advanced treatments or are difficult to heal. If amputation is required due to extensive tissue damage, they will assist to ensure proper wound healing is obtained and maintained.
Child Life Specialists help children deal with extreme medical conditions and treatments. They may assist in treatments to distract the child from what is going on and to help them navigate the world with changes in function and appearance.
Recreational Therapists assist with the adaption of sports or hobbies to your new function. They may introduce you to new sports and team sports.
Research
Sepsis research abounds in three main areas. These are the prediction and prevention of sepsis, the treatment of sepsis in the human body including at the cellular level, and recovery and rehabilitation.
Studies are conducted to avoid the development of sepsis by understanding how it occurs. It is thought that there is a disconnection in the inflammatory response but how this occurs is not certain. Internal body inflammation also is a key to understanding the evolution of sepsis in the body. The study of biomarkers which are body substances that change with certain diseases is also of interest in the prediction and prevention of sepsis.
The Surviving Sepsis Campaign (SSC) is a consortium of scientists that work together to develop guidelines, bundles, and clinical protocols for the prevention, diagnosis, and treatment of sepsis. In addition to the many scientists and researchers around the world working individually on specific aspects of sepsis, the consortium reviews studies using evidence-based strategies for the care of individuals with sepsis. They utilize research from around the world.
Recovery and rehabilitation strategies come from all aspects of healthcare. Neurological, cardiac, pulmonary, liver, kidney, vascular, orthopedics, and many other scientific discoveries are used in the treatment of sepsis and post-sepsis conditions. This research is being conducted by scientists, physicians, nurses, therapists, mental health professionals as well as others in the healthcare field. Specific clinical trials and research study information can be found by searching the word ‘sepsis’ on this website.
Facts and Figures
The Centers for Disease Control and Prevention (CDC) released these figures about sepsis:
- 7 million adults in America develop sepsis every year
- 270,000 individuals die of sepsis in the U.S. every year
- 1 in 3 hospital deaths involved sepsis every year
- 87% of cases of sepsis start outside of the hospital (CDC, 2020)
Most individuals recover from a mild case of sepsis. Recovery from severe sepsis or septic shock is about 40 percent.
Septic shock occurs in about 15% of sepsis cases. Most deaths occur in individuals in the ICU.
The annual cost of sepsis in the U.S. is $20.3 billion per year.
Resources
If you are looking for more information about sepsis or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309.
Additionally, the Reeve Foundation maintains fact sheets on a wide variety of paralysis-related topics ranging from state resources to secondary complications of paralysis.
We encourage you to also reach out to organizations that provide sepsis information including:
Centers for Disease Control and Prevention
Clinical Guidelines provide evidence-based treatment protocols for healthcare professionals:
Centers for Disease Control and Prevention, Clinical Tools
Sepsis and Septic Shock: Guideline-Based Management: Siddharth Dugar, Chirag Choudhary, Abhijit Duggal. Cleveland Clinic Journal of Medicine Jan 2020, 87 (1) 53-64; DOI: 10.3949/ccjm.87a.18143
Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021: Evans, L. et al. Critical Care Medicine: November 2021 – Volume 49 – Issue 11 – p e1063-e1143 doi: 10.1097/CCM.0000000000005337
Surviving Sepsis Campaign, Pediatric Patients
References
Ackerman MH, Ahrens T, Kelly J, Pontillo A. Sepsis. Crit Care Nurs Clin North Am. 2021 Dec;33(4):407-418. doi: 10.1016/j.cnc.2021.08.003. Epub 2021 Oct 9. PMID: 34742497.
Anderson D, Kutsogiannis DJ, Sligl WI. Sepsis in Traumatic Brain Injury: Epidemiology and Outcomes. Can J Neurol Sci. 2020 Mar;47(2):197-201. doi: 10.1017/cjn.2019.320. PMID: 31659951.
Barichello T, Generoso JS, Singer M, Dal-Pizzol F. Biomarkers for Sepsis: More Than Just Fever and Leukocytosis-a Narrative Review. Crit Care. 2022 Jan 6;26(1):14. doi: 10.1186/s13054-021-03862-5. PMID: 34991675; PMCID: PMC8740483.
Downes KJ, Fitzgerald JC, Weiss SL. Utility of Procalcitonin as a Biomarker for Sepsis in Children. J Clin Microbiol. 2020 Jun 24;58(7):e01851-19. doi: 10.1128/JCM.01851-19. PMID: 32350044; PMCID: PMC7315022.
Fernández-Sarmiento J, de Carvalho WB. Bundle for Pediatric COVID-19 Sepsis. Rev Assoc Med Bras (1992). 2021 Jul 9;67Suppl 1(Suppl 1):26-28. doi: 10.1590/1806-9282.67.Suppl1.20200714. PMID: 34259765.
Filetici N, Van de Velde M, Roofthooft E, Devroe S. Maternal Sepsis. Best Pract Res Clin Anaesthesiol. 2022 May;36(1):165-177. doi: 10.1016/j.bpa.2022.03.003. Epub 2022 Mar 30. PMID: 35659952.
Gauer R, Forbes D, Boyer N. Sepsis: Diagnosis and Management. Am Fam Physician. 2020 Apr 1;101(7):409-418. PMID: 32227831.
Jaja BNR, Jiang F, Badhiwala JH, Schär R, Kurpad S, Grossman RG, Harrop JS, Guest JD, Toups EG, Shaffrey CI, Aarabi B, Boakye M, Fehlings MG, Wilson JR. Association of Pneumonia, Wound Infection, and Sepsis with Clinical Outcomes after Acute Traumatic Spinal Cord Injury. J Neurotrauma. 2019 Nov 1;36(21):3044-3050. doi: 10.1089/neu.2018.6245. Epub 2019 Jun 17. PMID: 31007137; PMCID: PMC6791472.
Jones TW, Smith SE, Van Tuyl JS, Newsome AS. Sepsis with Preexisting Heart Failure: Management of Confounding Clinical Features. J Intensive Care Med. 2021 Sep;36(9):989-1012. doi: 10.1177/0885066620928299. Epub 2020 Jun 4. PMID: 32495686; PMCID: PMC7970342.
Jyoti A, Kumar S, Kumar Srivastava V, Kaushik S, Govind Singh S. Neonatal Sepsis at Point of Care. Clin Chim Acta. 2021 Oct;521:45-58. doi: 10.1016/j.cca.2021.06.021. Epub 2021 Jun 18. PMID: 34153274.
Kosyakovsky LB, Angriman F, Katz E, Adhikari NK, Godoy LC, Marshall JC, Ferreyro BL, Lee DS, Rosenson RS, Sattar N, Verma S, Toma A, Englesakis M, Burstein B, Farkouh ME, Herridge M, Ko DT, Scales DC, Detsky ME, Bibas L, Lawler PR. Association Between Sepsis Survivorship and Long-Term Cardiovascular Outcomes in Adults: a Systematic Review and Meta-Analysis. Intensive Care Med. 2021 Sep;47(9):931-942. doi: 10.1007/s00134-021-06479-y. Epub 2021 Aug 9. PMID: 34373953.
Kumar S, Theis T, Tschang M, Nagaraj V, Berthiaume F. Reactive Oxygen Species and Pressure Ulcer Formation after Traumatic Injury to Spinal Cord and Brain. Antioxidants (Basel). 2021 Jun 24;10(7):1013. doi: 10.3390/antiox10071013. PMID: 34202655; PMCID: PMC8300734.
Levy, Mitchell M. MD, MCCM1; Evans, Laura E. MD, MSc, FCCM2; Rhodes, Andrew MBBS, FRCA, FRCP, FFICM, MD (res)3. The Surviving Sepsis Campaign Bundle: 2018 Update. Critical Care Medicine: June 2018 – Volume 46 – Issue 6 – p 997-1000. doi: 10.1097/CCM.0000000000003119
L’Heureux M, Sternberg M, Brath L, Turlington J, Kashiouris MG. Sepsis-Induced Cardiomyopathy: a Comprehensive Review. Curr Cardiol Rep. 2020 May 6;22(5):35. doi: 10.1007/s11886-020-01277-2. PMID: 32377972; PMCID: PMC7222131.
Lin H, Chen H, Qi B, Jiang Y, Lian N, Zhuang X, Yu Y. Brain-Derived Extracellular Vesicles Mediated Coagulopathy, Inflammation and Apoptosis After Sepsis. Thromb Res. 2021 Sep 23;207:85-95. doi: 10.1016/j.thromres.2021.09.014. Epub ahead of print. PMID: 34583153.
Meneses G, Cárdenas G, Espinosa A, Rassy D, Pérez-Osorio IN, Bárcena B, Fleury A, Besedovsky H, Fragoso G, Sciutto E. Sepsis: Developing New Alternatives to Reduce Neuroinflammation and Attenuate Brain Injury. Ann N Y Acad Sci. 2019 Feb;1437(1):43-56. doi: 10.1111/nyas.13985. Epub 2018 Nov 29. PMID: 30499145.
Mok G, Hendin A, Reardon P, Hickey M, Gray S, Yadav K. Macrocirculatory and Microcirculatory Endpoints in Sepsis Resuscitation. J Intensive Care Med. 2021 Dec;36(12):1385-1391. doi: 10.1177/0885066620982585. Epub 2020 Dec 30. PMID: 33375916.
Pierrakos C, Velissaris D, Bisdorff M, Marshall JC, Vincent JL. Biomarkers of Sepsis: Time for a Reappraisal. Crit Care. 2020 Jun 5;24(1):287. doi: 10.1186/s13054-020-02993-5. PMID: 32503670; PMCID: PMC7273821.
Pleşa-Furda P, Iancu I, Cioltean C, Breazu C, Brinzilă S, Odaini A, Bocşe H, Herdean A, Bartoş D, Turculeţ C, Iancu C, Bartoş A. Abdominal Sepsis – Current Definitions and Practice. Chirurgia (Bucur). 2021 Dec;116(6 Suppl):S16-S27. PMID: 35274608.
Purcarea A, Sovaila S. Sepsis, a 2020 Review for the Internist. Rom J Intern Med. 2020 Sep 1;58(3):129-137. doi: 10.2478/rjim-2020-0012. PMID: 32396142.
Salomão R, Ferreira BL, Salomão MC, Santos SS, Azevedo LCP, Brunialti MKC. Sepsis: Evolving Concepts and Challenges. Braz J Med Biol Res. 2019;52(4):e8595. doi: 10.1590/1414-431X20198595. Epub 2019 Apr 15. PMID: 30994733; PMCID: PMC6472937.
Simonsen KA, Anderson-Berry AL, Delair SF, Davies HD. Early-Onset Neonatal Sepsis. Clin Microbiol Rev. 2014 Jan;27(1):21-47. doi: 10.1128/CMR.00031-13. PMID: 24396135; PMCID: PMC3910904.
Rhee C, Chiotos K, Cosgrove SE, Heil EL, Kadri SS, Kalil AC, Gilbert DN, Masur H, Septimus EJ, Sweeney DA, Strich JR, Winslow DL, Klompas M. Infectious Diseases Society of America Position Paper: Recommended Revisions to the National Severe Sepsis and Septic Shock Early Management Bundle (SEP-1) Sepsis Quality Measure. Clin Infect Dis. 2021 Feb 16;72(4):541-552. doi: 10.1093/cid/ciaa059. PMID: 32374861; PMCID: PMC8189682.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit Care Med. 2017 Mar;45(3):486-552. doi: 10.1097/CCM.0000000000002255. PMID: 28098591.
Sabih A, Leslie SW. Complicated Urinary Tract Infections. 2022 May 27. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 28613784.
Sekino N, Selim M, Shehadah A. Sepsis-Associated Brain Injury: Underlying Mechanisms and Potential Therapeutic Strategies for Acute and Long-Term Cognitive Impairments. J Neuroinflammation. 2022 Apr 29;19(1):101. doi: 10.1186/s12974-022-02464-4. PMID: 35488237; PMCID: PMC9051822.
Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017 Mar;43(3):304-377. doi: 10.1007/s00134-017-4683-6. Epub 2017 Jan 18. PMID: 28101605.
Vandewalle J, Libert C. Glucocorticoids in Sepsis: To Be or Not to Be. Front Immunol. 2020 Jul 21;11:1318. doi: 10.3389/fimmu.2020.01318. PMID: 32849493; PMCID: PMC7396579.
Weiterer S, Frick S, Lichtenstern C, Hug A, Uhle F, Weigand MA, Hundt G, Siegler BH. Sepsis in Mechanically Ventilated Patients with Spinal Cord Injury: A Retrospective Analysis. Spinal Cord. 2019 Apr;57(4):293-300. doi: 10.1038/s41393-018-0217-5. Epub 2018 Nov 9. PMID: 30413803; PMCID: PMC6477786.
Woźnica EA, Inglot M, Woźnica RK, Łysenko L. Liver Dysfunction in Sepsis. Adv Clin Exp Med. 2018 Apr;27(4):547-551. doi: 10.17219/acem/68363. PMID: 29558045.
Zhang YY, Ning BT. Signaling Pathways and Intervention Therapies in Sepsis. Signal Transduct Target Ther. 2021 Nov 25;6(1):407. doi: 10.1038/s41392-021-00816-9. PMID: 34824200; PMCID: PMC8613465.