Cerebral Palsy
In the 1860s an English doctor, William Little, wrote about a condition of stiff legs and arms in children. This is the first documentation of cerebral (brain) palsy (muscle weakness). Today there is much more known about cerebral palsy (CP) and how to provide rehabilitation therapies to enhance function.
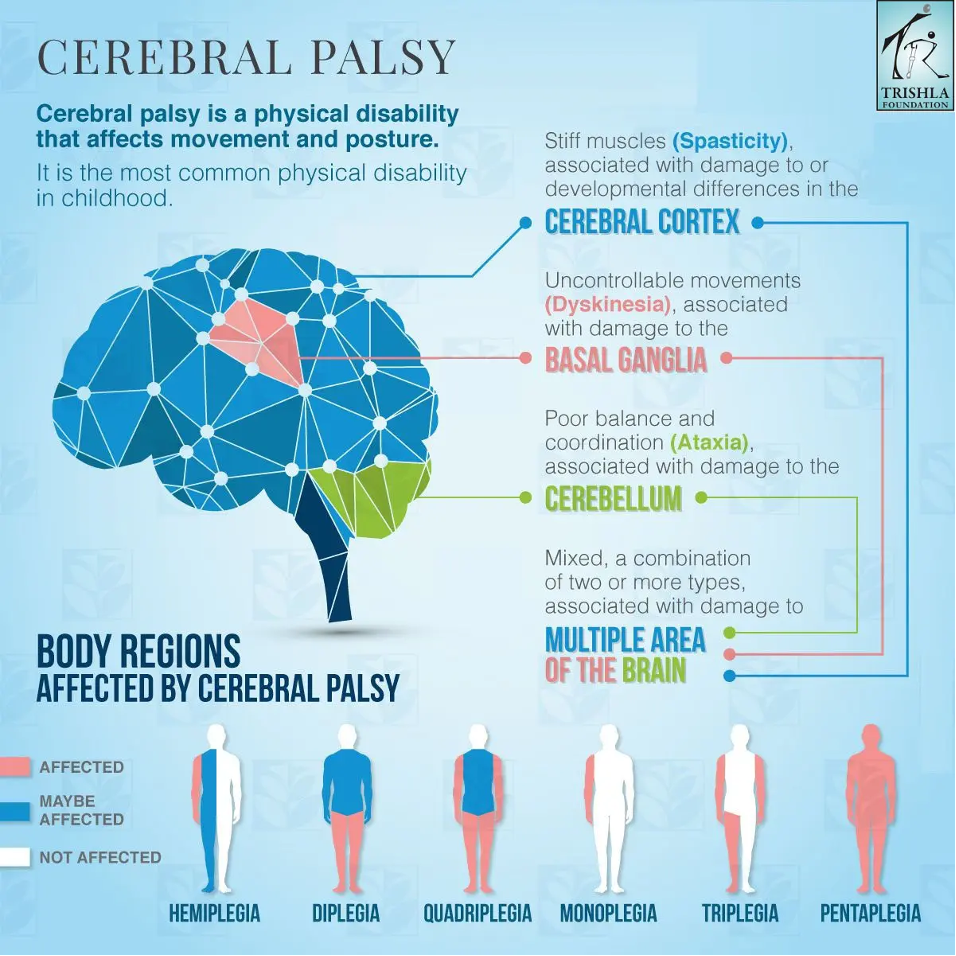
Cerebral palsy includes issues of movement, posture, and muscle tone with onset before, during, or shortly after birth. However, there are distinct categories of metabolic (internal body functions) and genetic (inherited) disorders. Cerebral palsy can result in general mentation and physical dysfunction or isolated issues with gait, cognition, growth, or sensation.
It is important to note that CP is not a progressive diagnosis. This means that the condition does not worsen over time. Most individuals with CP have normal to above average intellect. Life expectancy is the same for individuals with CP as for those without CP.
The majority of individuals with CP have tone or spasticity. This occurs because the cell bodies of the upper motor neurons (the nerves that send movement messages from the brain to the body) are located in the brain. Since CP affects the brain, the upper motor neurons can become hyperactive, sending too many messages without relaxation through the nerves to the muscles resulting in tone or spasticity.
There are four main types of cerebral palsy:
Spastic Cerebral Palsy is increased muscle tone (spasticity). It affects the cerebral cortex of the brain where a part of voluntary movement is controlled. This is the most common form of CP affecting about 80% of individuals with CP. There are three types of spastic cerebral palsy:
- Spastic diplegia/diparesis consists of muscle tone or stiffness mostly in the legs with the arms less affected or not at all. Walking can be an issue due to increased tone.
- Spastic hemiplegia/hemiparesis affects just one side of the body with the arm being more affected by tone than the leg.
- Spastic quadriplegia/quadriparesis involves the arms, legs, trunk, and face which can affect oral motor function such as speech and eating. Intellectual challenges, seizures, vision, hearing, and walking can be challenged.
- Dyskinetic Cerebral Palsy involves issues controlling fast or slow movement of hands, arms, feet, and legs. The face and tongue may also be involved. About 70% of individuals have lesions in varying locations throughout the brain. Activities such as sitting, walking, swallowing, and talking can be affected. Subsets of dyskinetic cerebral palsy include:
- Athetoid consists of involuntary movements anywhere in the body that can be hypertonic (very fast) or hypotonic (vary slow). These speeds vary within the individual.
- Choreoathetoid is a combination of sluggish movements mostly in the fingers and face and sudden movements especially in the fingers and toes.
- Dystonic cerebral palsies are slow, rotational movement of the torso, arm or leg or combination of these body parts.
- Ataxic Cerebral Palsy affects muscle coordination particularly in the legs and arms. This occurs from damage to the cerebellum, which is the part of the brain that controls muscle function. It occurs in 5-10% of individuals with cerebral palsy. Affects include hypotonia (weak muscle tone), tremors, visual (seeing) and auditory (hearing) processing.
- Mixed Cerebral Palsy is a combination of the above types of CP. The most common type of mixed CP is spastic and dyskinetic, but any combination is possible.
 Reprinted by permission from the Trishla Foundation https://www.trishlafoundation.com/cerebral-palsy-complete-guide/
Reprinted by permission from the Trishla Foundation https://www.trishlafoundation.com/cerebral-palsy-complete-guide/
Congenital Cerebral Palsy
The causes of congenital (present from birth) CP include issues in brain development or injury to the brain. This form of CP can occur in utero, at birth or up to 28 days after birth. These issues can include:
- Damage to the part of the brain that send signals to the body.
- Abnormal brain development due to infection, fever, trauma, or genetic changes.
- Bleeding in the brain from stroke, bleeding in the brain, blood vessel malformation, blood clotting, heart issues, or sickle cell disease.
- Lack of oxygen in the baby’s brain from low maternal blood pressure, placenta detachment, constriction of the umbilical cord, or severe trauma.
Acquired Cerebral Palsy
A small number of individuals develop CP due to injury of the brain that occurs more than 28 days after birth. This is called acquired CP, and usually is associated with an infection (such as meningitis) or head injury. Acquired cerebral palsy develops 28 days after birth. Causes of acquired CP include some of the same issues as congenital causes such as infection from meningitis or encephalitis, lack of blood flow to the brain from cerebrovascular accidents (stroke in the baby), bleeding in the brain, blood vessel malformation, blood clotting, heart issues, or sickle cell disease. CP can also be acquired by infants due to trauma producing injury to the brain, including head injuries caused by motor vehicle crashes, dropped baby, shaken baby, or child abuse.
Risk Factors of Cerebral Palsy
The reason some children develop cerebral palsy is not known. There are risk factors but the presence of a risk factor, does not mean your child will develop CP. In fact, many individuals with these risk factors do not result in CP. Risk factors for CP include:
- Low birthweight of babies under 3 pounds, 5 ounces (1,500 grams) although it has been noted in babies less than 5 1/2 pounds (2,500 grams) at birth.
- Premature birth or babies born before the 32nd week of pregnancy or through to the 37th week.
- Multiple births, especially if one of the babies does not survive before birth or shortly after birth.
- Assisted reproductive technology (ART) infertility treatments is noted as a risk factor but not due to the ART process. It is because ART often involves two other risk factors, preterm delivery, and multiple births.
- Infections during pregnancy such as chicken pox, rubella (measles) or cytomegalovirus (CMV), bacterial infections, or pelvic infections. Even fevers during pregnancy can increase risk. This is because infections release cytokines (proteins) which cause inflammation within the body.
- Jaundice or too much bilirubin in the blood of the infant which turns the skin yellow. Left untreated, jaundice leads to kernicterus. Jaundice can be from bilirubin build up or blood type incompatibility.
- Medical conditions of the mother such as thyroid problems, intellectual disability, or seizures.
- Birth complications including detachment of the placenta, uterine rupture, or problems with the umbilical cord which can disrupt oxygen supply.
Symptoms of Cerebral Palsy
Anatomically, CP can affect muscles in structure and function. Force of muscle movement can be decreased. Range of motion can be limited. Muscles can be decreased in size, increased in length, and have a slightly different composition. There are generally fewer muscle stem cells to enhance growth as well as to repair or replace ongoing muscle tissue.
The physical symptoms of CP are variable. The symptom will correlate with the location of injury to the brain. Not every child will have all symptoms. The level of involvement of symptoms also varies by individual.
Movement
Tone (spasticity) is the most notable symptom of cerebral palsy as it occurs in about 80% of cases. Typically, tone will appear as spasming muscles or even rigidity, but it can also include lack of tone or floppy muscles.
Dystonia is uncontrolled movement. This can include jerky movements or tremors as well as slow, writhing movements.
Due to brain injury, movement, posture and balance are the most affected functions. One side of the body may be used more than the other. Difficulty with walking may include a wide, asymmetrical, scissors gait, or walking on the toes. Fine motor skills such as writing, eating, buttoning, or zipping may be affected.
Secondary physical conditions can develop due to complications of tone including hip pain or dislocation, hand dysfunction, and foot drop where the foot cannot be pulled up into a neutral position (equinus deformity). If tone becomes overwhelming, contractures (shortening of muscles usually around a joint) can occur. Osteopenia (in which your bones become weaker than normal) and osteoporosis can develop from lack of weight through bones. Fractures (broken bones) can occur from poor bone density and movement against contractures. Scoliosis or other spinal issues can develop due to muscle imbalances.
Pressure injury can occur from sitting without pressure release, from equipment rubbing against the skin or from tone (spasms) of skin rubbing against something.
Oral Motor
Nutrition issues can occur due to feeding difficulties of arm mobilization to bring the food to the mouth and oral motor issues for chewing and swallowing, drooling and difficulty in communication. Tone (spasticity) can occur within the body creating gastrointestinal issues, bowel obstruction, vomiting and constipation. Gaining weight may be a challenge.
Development
Physical growth may be delayed. The individual may be smaller in stature than other children or adults. Developmental milestones may be slower to be reached. Adaptations to milestones may need to be modified such as independence in wheelchair mobility vs. walking.
Learning and intellectual difficulties may be present. Cognitive dysfunction might include issues of perceiving, acquiring, understanding, and responding to information. This can affect thoughts, memory, and problem solving. It may include issues with attention or executive functions (higher level thinking).
Emotional disorders and behavioral problems are sometime present due to chemical issues within the brain or mental health challenges from depression or social isolation.
Sensory
Individuals with CP may have sensory issues. This can include visual impairment and difficulty controlling eye movement. Hearing can be affected. Some can have decreased or heightened sensations for pain and touch sensitivity. Feeling pressure on the skin can be heightened or decreased.
Seizures
Seizures are sudden explosions of electrical impulses from the brain. These can range from staring into space to jerking body movements. Behavioral or emotional issues can be present. Speech and hearing impairment can be present. Vision can be affected most often due to crossed eyes. Incontinence of bowel and bladder can be present. Later in life, sexual development may be delayed.
Bladder and Bowel Function
Bladder function may be affected due to functional incontinence which is when an individual inadvertently releases urine because of limitations in communicating the need to urinate, urgency, an inability to get to the toilet in time, to be able to remove clothing, or slow response by a caretaker. Neurological causes of bladder incontinence include neurogenic bladder (miscommunication of bladder needs by the nerves of the body) or spasms in the bladder which force urine out.
Constipation is an issue for individuals who have difficulty eating, chewing, and moving stool through the body due to neurogenic bowel (a slowing of the bowel due to miscommunication of bowel function by the nerves of the body), slow functioning bowel, or stimulation of the bowel due to lack of body movement (mobility and exercise).
Diagnosis of Cerebral Palsy
Prompt diagnosis of cerebral palsy is critical to early intervention strategies. You may not notice signs of CP in a newborn. Maintaining newborn and childhood checkups are critical to early diagnosis. Following developmental milestones can provide an indication of concerns.
Cerebral palsy might first be noted by physical examination. This includes a history looking for risk factors of early delivery, respiratory distress syndrome (RDS), premature birth, brain hemorrhage, sepsis, meningitis, hydrocephalus, and seizures. A physical examination can detect increases or decreases in tone (spasticity). The type of CP is diagnosed by symptoms.
Some symptoms of CP may not appear until age two when motor development is lagging behind the child’s peers.
Testing includes MRI (magnetic resonance imaging) to examine the brain if the physical examination is unclear. Infants and young children will be given a sedation for comfort during the procedure and to ensure they are still.
A cranial ultrasound may be done to view the general anatomy of the brain, but this does not provide the same degree of specifics as the MRI.
There is no blood test for cerebral palsy.
Evaluation of Cerebral Palsy
There are several measurement instruments used to assess individuals with cerebral palsy. The choice of assessments is based on the needs of the individual. Other assessment instruments may be used by different facilities. Progress is observed by use of the same instruments over time. If you move or change healthcare providers, you may need to ask about using the same instrument. Assessments typically include sleep, mental and/or psychosocial function, behavior. and physical abilities. Traditional developmental skills assessments are also used. The most commonly used assessments are:
The Gross Motor Function Classification System (five levels for ages 0-12) is a measurement of physical abilities used to evaluate individuals with CP as well as their response to treatment. The instrument is helpful in selecting therapy techniques.
The Communication Function Classification System measures everyday sending and receiving communication with known and unknown individuals.
The Manual Ability Classification System (for ages 4-18) provides information about handling objects which can help establish therapy needs as well as assistance in school.
Treatment of Cerebral Palsy
The care provided for individuals with CP is in response to their symptoms. Each treatment plan is based on the individual’s specific needs. Ensuring independence is the goal of treatment. Several approaches to one issue may be used.
Movement
Tone (spasticity) Movement issues are often present in individuals with CP. Tone (spasticity) is the primary issue in CP for most individuals. Reduction of tone can avoid many complications, will make the individual more comfortable and able to function more independently.
Some with mild (tone) spasticity may use it to assist with transfers and standing. Treatment for using tone to enhance function is typically not sought but still should be monitored for complications.
Medication may be used by those with significant tone to reduce tone (spasticity). Oral medication flows throughout the bloodstream affecting the entire body. These drugs include alpha2-adrenergic agonists, benzodiazepines, baclofen, dantrolene sodium, and gabapentin. They all have the side effect of sedation which may not be desired. Over time, the body will become accustomed to the medication without noticeable sedation. Typically, the oral medication will have to be increased as the body becomes accustomed to it.
An alternative to oral medication is Botox (onabotulinumtoxin A) which is injected just into the muscles with tone, thereby not affecting the whole body. This does require routine injections approximately every 4-6 months.
If tone is severe throughout the body, a pump is placed in the abdomen that is connected to a tube routed into the spinal fluid that delivers a continuous flow of high doses of liquid baclofen. If pain is an issue, pain medication can be added to the pump. This can relax the lower to mid upper body. Repeat fillings of the medication into the pump is done with injection through the abdominal skin. The pump can be adjusted using a magnetic device placed on the abdomen. A continuous dose of medication can be programed or boluses (dosages of drugs given intravenously) can be distributed over time during active times of the day.
Phenol injections have been used to block nerve transmission in individuals with tone. A 3% mixture of phenol is being used in some areas which is causing a temporary effect like Botox. Repeated injections are needed. Formerly, a 6% mixture was used which damaged the nerve causing it to lose function. The lower mixture preserves the nerve but has a temporary effect.
Selective dorsal rhizotomy is a neurosurgical procedure that includes electromyography (EMG)/nerve conduction studies (NCS) directly to the nerves during surgery. The nerves fibers (not the entire nerve) with hyper tone are interrupted from message transmission thereby reducing tone. This surgical procedure can take many hours to complete.
Contractures are a complication of lack of movement. Some individuals do not move their joints to keep them supple from lack of ability due to tone (spasticity). Muscles have a balance between those that push and those that pull with the muscles drawing toward the body being just a bit stronger. The body, in its relaxed state, will draw itself into a fetal position. For some individuals, assistance is needed through range of motion exercises or gentle stretching to move the muscles in all the directions that specific muscle moves. If this is not done, the muscle become out of balance.
Orthopedic Surgeries are used depending on the need. Manual moving of a contracted muscle can tear or injure the muscle that is stiff and shortened. Repeated casting or braces can be used to very slowly re-stretch the muscle to its functional use. If tone is present, medications or injections can be used to help relax the muscle. Soft tissue releases can reduce contractures. If contractures are too severe or pull a joint out of position, an orthopedic surgery may be needed to surgically release the muscle.
Tendon transfers are the surgical moving of tendons from one area to another to increase strength.
Scoliosis is an orthopedic condition where the bones of the spinal column are pulled out of alignment due to an imbalance of muscles in the back. This is often a consequence of tone (spasticity). Use of positioning equipment in sitting and laying can assist in avoiding this complication. However, occasionally, the tone becomes too strong resulting in the muscle imbalance. If the vertebrae are pulled too severely, the spinal cord can become damaged. However, scoliosis is typically diagnosed early. Oral medications or Botox injections can reduce tone restoring muscle balance in the early stages. In some cases, surgery is done placing rods along the spine to support it.
Strength training can be undertaken by anyone who wants to improve their general health. For some individuals this might include general body building. It also includes strengthening specific muscles or muscle groups. For instance, if a contracture or scoliosis is in an early forming stage, building strength in the opposing muscle group can reduce the risk of developing a complication.
Mobility may be a desired function. There are many therapies which can assist in attempting to establish this goal. Use of high-top athletic shoes or walking boots for ankle support, braces, crutches, a reverse walker, manual or powerchair can accomplish this goal. The individual may propel independently or use adaptions to move their chair with power assist to wheels, one arm drive, or sip and puff with their mouth. Some mobility devices are moved with the feet like a bike instead of with the arms.
Balance and coordination exercises first need to be mastered if walking is a goal. Strengthening in the legs, trunk and arms to hold the body erect should be accomplished. Techniques such as parallel bars, weight supported walking using a harness to support the body, and treadmills are just a few techniques that might be utilized. Use of adaptive equipment such as bracing, a walker or other stabilizing equipment might be used.
Oral Motor
Oral sensorimotor therapy is a method to stimulate oral motor function for eating and improvement in drooling. This therapy may include desensitization or stimulation based on need. Specific therapies might include oral sensorimotor management, positioning, oral appliances, food thickeners, specialized formulas, and neuromuscular stimulation. Neuromuscular stimulation includes rubber devices with varying texture tips to adjust to different textures. Arm support equipment can improve feeding independence.
Barium swallow is a radiographic test of the ability to safely swallow. While a barium drink is provided, an X-ray of the individual swallowing it is taken. The examiner will be able to determine if the swallowing mechanism is working correctly and that food or fluid is not entering the lungs.
Caloric intake is imperative to growth and development. In some cases, a feeding tube placed through a surgical opening in the abdomen to the stomach can provide the nutrition needed. Dietitians or healthcare nutritionists can provide a diet and caloric plan.
Learning to control motor function of the mouth, tongue, and throat can improve swallowing and speech. There may be no speech dysfunction, dysphonia due to breathing, tone (spasticity) or other motor issues. Most individuals accomplish conversational speech without adaptions or with therapy. Some might opt for computer programs that will speak for them. They may type their thoughts, have frequently used phases at the ready, or use eye or head-controlled technology to make their needs known.
Dental hygiene and support are critical to the individual with cerebral palsy to ensure an aligned bite and chewing ability. Tone (spasticity) can pull the jaw out of alignment or make mouth closure difficult. Getting nutrition into the body, and chewing are the start to nutritional support.
Development
Developmental monitoring, screening and medical evaluations are all critical to following the progress your child is making. Interventions are established to assist in providing your child with the best outcomes. Cerebral palsy is not a progressive disease meaning it does not worsen over time, but you can structure the individual’s abilities and environment for success.
Exercise or movement to the body is critical for everyone. For individuals who have issues with moving the body, all body joints should be moved for them daily. Finding activities that encourage movement is essential. Incorporating play into movement makes accomplishing this goal easier for smaller children.
School is the work of children. There is assistance for establishing a functional learning environment. The Individual Educational Plan (IEP) is a document that is developed with school personnel. Input from your medical professional is helpful. Your knowledge about the wants and needs of your student is imperative. The plan is a written document that will allow all school personnel to know what is needed to provide your student with success.
Aquatic therapy is used to learn movements using the buoyancy of the water to assist. This reduces gravity as a limiting factor. When moving slowly in the water, gentle movements with little resistance can be learned. These movements are then transferred into functional gains out of the water.
A heated pool helps with relaxing the body muscles to facilitate movement. A certified pool therapist will be able to harness movements appropriately. Swim diapers are typically required.
Constraint-induced therapy is a technique where an individual is challenged to use their less active limb by restricting use of the opposite more active limb. This encourages use of both sides of the body which can increase function.
Sensory
Visual impairment can occur from the same issues as anyone who needs vision correction. In CP, it can also occur from the muscles of the eyes being pulled out of alignment due to tone (spasticity) or nerve impairment. An ophthalmologist is important to assessing overall vision. Treatments range from glasses to Botox injections to reduce eye muscle spasms, to a patch covering the more active eye which forces the less active eye to be more functional.
Hearing is affected by nerve function. If the nerves to the ears are affected by CP, hearing can be a challenge.
Body sensation can be low or high throughout the body. Stimulation therapies using different advancing textures can assist with sensitivity. For those with decreased sensation, pressure releases or moving of the body weight off boney prominences is critical to reduce the risk of pressure injury.
Pressure Injury can occur due to lack of sensation as well as lack of movement. Not being able to adjust the body due to mobility challenges can lead to skin breakdown especially over boney prominences or from equipment rubbing against the skin. Pressure injury begins inside the body where you cannot see the tissue damage. The first sign of pressure injury is a change in pigmentation on the surface of the skin, usually over a prominent bone such as the hip, sitting bones or sacrum. In darkly pigmented individuals, the area may first appear as a purple or ashy spot. In lightly pigmented individuals the spot may appear as a red area. Any area where a bone protrudes is a risk area.
Pressure injury is measured in stages. Stage one is a spot on the skin. In stage two the surface of the skin is eroded which creates an opening in the skin. Stage three consists of a deep wound into the inner tissue. In stage four the wound is open to the bone. An unstageable wound has a crust on the opening or within the opening so the depth of the wound cannot be visualized.
Treatments for pressure injury includes prevention by use of pressure dispersing equipment and pressure releases. If a change in pigmentation is seen, the area should not have any pressure until the pigmentation reverts to the individual’s normal color. Wounds at any stage should be evaluated for appropriate treatment.
Friction and shearing injury should also be noted. These occur when the layers of skin are separated, similar to a rug burn. As children like to free form on the floor for play and activities, friction and shearing injuries can happen quickly. If there is a risk from free form or equipment rubbing, always check to make sure the skin is intact and use long pants and long sleeve shirts to protect from these injuries.
Hippotherapy uses the movement of a horse at the walk to improve sensory, neuromotor and cognitive functions. The gentle sway of the movement allows the individual to gain function in a calm environment. Plus, people love it. It is important to have a therapist (occupational therapist, physical therapist or speech language pathologist) who specializes in hippotherapy to perform the therapy for best results. There are techniques specifically designed to gain benefits.
Seizures
Seizures can be common in individuals with cerebral palsy. A seizure is an electrical burst of energy in the brain that can affect orientation and movement. Some individuals with CP do not have seizures, some have a few over a lifetime and others have seizures more often. It is important to be able to discriminate between seizures and rhythmic tone (spasticity) as they are different.
Depending on the location of injury to the brain, partial seizures can occur affecting part or all of the body, auditory hallucinations, sensory and thinking issues. These seizures can be brief or longer lasting.
Absence seizures appear as a staring look with the eyes usually looking up. In some, the eyelids will flutter, and there may be lip smacking or chewing motions. The child will not respond. These last for about 20 seconds. When resolved, the child continues whatever activity they were doing without awareness of the seizure. These seizures often resolve in early adulthood.
Myoclonic seizures present with jerking of just a part of the body, one or both arms or legs, torso, or face. They last only seconds. Awareness may be lost but since the seizure is so brief, it is difficult to assess. This type of seizure is easily confused with tone (spasm) but you will learn to discriminate the movements in your own child.
In atonic seizures, all muscle tone and consciousness is lost for a few minutes, but jerking body movements are not present. Falling is a risk in this type of seizure. Helmets may be needed to protect from head injury. This type of seizure can happen multiple times a day.
Tonic-clonic seizures involve repetitive body movements and loss of consciousness. This is a severe seizure that is familiar to most individuals. Breathing can be affected. Position the individual on their left side in a safe area so their body is not injured and DO NOT PUT ANYTHING IN THEIR MOUTH. This type of seizure can last several minutes. Recovery is needed due to exhaustion and to reorient to surroundings.
Diagnosis of seizures is done by EEG (electroencephalogram). Electrodes are placed on the skin of the head to detect the area of electrical disturbance. The best information is obtained during the seizure, but information can be obtained after a seizure while the brain is recovering.
Anti-convulsant medications are used to treat seizures. If seizures continue, a ketogenic diet may be used but it is critical that this should be attempted only under the direction of a healthcare provider. Severe cases of seizures may be treated by surgical intervention to either remove or interrupt the seizure activity.
Bowel and Bladder Function
Bladder function can be affected by cerebral palsy in a variety of ways. Urinary incontinence can be present due to functional issues of not being able to adjust clothing in time as well as the inability to transfer to the toilet. Incontinence can occur from the amount of time needed to respond to the urge to void or in getting assistance to do so. A timing schedule assists with planned toilet times to ensure continence. Males might opt for an external catheter.
If there is a neurological issue with urine elimination, an intermittent catheterization (IMC OR IC) program should be undertaken to ensure continence and to avoid damage to the kidneys from urine reflux. Urodynamic studies determine issues of neurogenic bladder including bladder contraction, urinary sphincter pressure and pressure in the lower urinary system. Spasticity can affect internal organs as well as what is seen on the outside of the body. Medications or Botox injections can assist with treatment. Males may benefit from a sphincterotomy (a small relaxation of the urinary sphincter) for long term kidney protection. This does result in urinary incontinence that is controlled by an external catheter. If intermittent catheterization is required, the Mitrofanoff procedure may be done especially for the convenience of females. In this procedure, a small opening through the navel is linked to the bladder. Intermittent catheterization is performed through this opening. No collection device is needed. Another alternative is a suprapubic catheter, an opening in the skin in the abdomen over the area of the bladder is performed but the catheter is left in the body.
Bowel continence is a concern for both incontinence and constipation. Functional bowel issues can be caused by an inability to manage clothing or to transfer to the toilet in time. A timed bowel program may assist with functional incontinence.
Constipation is an issue due to poor nutritional intake or a slow-moving bowel from body inactivity, or tone (spasticity) in the bowel. Neurogenic bowel or the nerves affecting bowel function can also be present. These issues are met with the use of a bowel program using a gentle suppository on a regular schedule every other day or daily. Adding activity and movement either by actively moving the body or having someone move the body will also assist in bowel motility.
Transitioning
A supportive environment is essential for all individuals. An issue for parents or guardians is to ensure your child is able to transition to adulthood. Since parents and guardians are the individuals who know the most about their child and care for them throughout childhood, it can be a challenge to prepare them to function in the adult world on their own. This is a challenge for all parents but particularly when you have been the advocate and main care provider. It is as much a part of the child’s life as your own.
Transitioning begins in early childhood with allowing the child to make age-appropriate decisions and choices. Like all children, let them begin by making easy choices such as which book to read and what clothes to wear. Slowly ease the child into self-care activities by explaining what you are doing, then let them take over as appropriate. Children go to school, which is nonnegotiable but other things such as after school activities can be their choice. Advance in the teen years. Keep the child informed at an age-appropriate level about their healthcare needs.
Make time for yourself and your partner for your own time. Coordinating your child’s life can become all consuming (this can happen to any parent) but be sure to consider your needs and desires for your life. The goal is to launch a child into adulthood. You need a life to be there for yourself when this occurs.
Respite care is an alternative to full time caretaking. Consider an individual or facility that you trust for a time to relax and decompress. It can benefit both the individual with CP as a source of new opportunities and independence as well as the parent. Many locations have day or overnight camps in the summer particularly for this purpose.
The Habilitation/Rehabilitation Healthcare Team
In pediatrics, children have not yet learned developmental skills, so habilitation or original learning developmental skills with adaptions are taught. Teens and adults undergo rehabilitation because they are relearning previously acquired skills.
The parent or guardian should be considered one of the main team members for the individual with cerebral palsy until the child becomes an adult. The parent or guardian spends the most time with the child thus they know the child’s life goals, likes and dislikes and the nuances of their concerns and issues. They should help create a plan for transition into adulthood with the support of the rehabilitation team.
Primary care physicians, pediatricians, or nurse practitioners should have advanced education in the care of an individual with cerebral palsy. This person manages the general health of an individual.
Physiatrists or rehabilitation specialists will manage the overall habilitation or rehabilitation of the child or adult with CP. A physiatrist is a physician who specializes in physical medicine and rehabilitation.
Specialty physicians will be brought to the team as needed. This may include a neurologist for movement and seizure control, orthopedic specialist for bone and muscle issues, neurosurgeon if nerve or brain surgery is elected.
Gastroenterologists are physicians that specializes in stomach and bowel issues to keep the gut healthy and maintain nutrition.
Urologists are physicians who can assess the urinary system to keep the kidneys healthy and to develop and maintain continence.
Ophthalmologists are specialists in eye care. This individual will ensure the safety and function of eyes.
Pediatric Dentists and Dentists will make sure your child’s bite is correct and maintain oral health.
Physical Therapy is used to assist with learning gross motor skills used in daily life such as transfers and walking. Techniques to reduce spasticity are used as well as strength building to improve functional ability.
Occupational Therapy is provided to assist with fine motor skills for example, feeding, grooming, and writing.
Dietitians can provide the number of calories and nutrients needed for growth and development based on activity level.
Rehabilitation Nurses can help teach medical management skills, medication regimens, bladder and bowel programs as well as incorporate treatments into daily life.
Child life specialists are individuals generally based in a hospital setting that create time for play and diversion from medical treatments. They help children cope with the challenges of hospitalization, and disability or chronic illness.
Teachers, principals, guidance counselors, and school nurses are important figures in planning the education opportunities that are tailored to the needs of your child for success in education. They, along with the individual and their parents or guardians are key in developing an individual educational plan (IEP) to provide the structure and environment to support your child’s education.
Adaptive technologists may become involved with environmental adaptions that will increase function and independence.
Research
The advancement of research into treatments for cerebral palsy is rapid. Issues of prevention of CP, medical treatments and quality of life are being studied. Complications of CP are vastly being reduced due to research. Reduction of mortality from cardiovascular issues in individuals with CP has been successfully ongoing.
Although the reasons why some individuals develop CP is still being researched, the number of cases of CP remains about the same. However, the incidence in preterm infants has increased as the survial rate of low birthweight infants increases. More information about why some develop CP and others do not is still under investigation.
Early intervention treatments are evolving. Umbilical cord blood cell therapy is being evaluated in individuals with cerebral palsy. If you have been advised that your child may be born with CP, have their cord blood banked for future use. Studies indicate that cord blood which is rich in stem cells may be helpful in mobility, neuroprotection, and neuroregeneration.
Research specific to CP as well as other medical issues is being shared for improvements in treatment of spasticity, seizures, pressure injury, and other health concerns. Technological advances in adaptive equipment abounds.
Facts and Figures (from https://www.cdc.gov/ncbddd/cp/data.html)
The CDC reports cerebral palsy occurs in 1 out of 323 or 3/1000 live births. It is the most common childhood motor diagnosis.
CP occurs more frequently in pre-term or low birth weight babies.
Spasticity is the most common movement issue in 80% of cases.
Mild to severe hearing loss is affected in 30 to 50% of individuals with CP.
In individuals with CP, walking independently is proficient in 58.9%, use of a hand-held mobility device occurs in 7.8%, and there is limited or no walking in 33.3%.
Seizures occur in 42% of individuals identified with CP.
Of the individuals identified with CP, 7.5% also had autism spectrum disorder (ASD).
In adults, the incidence of ischemic heart disease, cerebrovascular disease, cancer, and trauma are higher in those with CP than without CP.
Most individuals with CP live long, fulfilling lives. The age span is equal for those who have CP compared to those who do not.
Resources
If you are looking for more information on cerebral palsy or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 9:00 am to 8:00 pm ET.
Additionally, the Reeve Foundation maintains a fact sheet on cerebral palsy with resources from trusted sources. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
We encourage you to also reach out to cerebral palsy support groups and organizations for individuals and families, including:
American Academy for Cerebral Palsy and Developmental Medicine (AACPDM )
Eunice Kennedy Shriver National Institute of Child Health and Human Development
March of Dimes Birth Defects Foundation
Clinical Guidelines
Agency for Healthcare Research and Quality (AHRQ). Evidence-Based Practice Center Comparative Effectiveness Review Protocol, Feeding and Nutrition Interventions in Cerebral Palsy https://www.christopherreeve.org/wp-content/uploads/2024/04/cerebral-palsy-feeding_research-protocol.pdf
Waikato District Health Board, Child Development Centre Therapy Team. Cerebral Palsy Clinical Practice Guideline CP-CPG. New Zealand, 2014. https://www.christopherreeve.org/wp-content/uploads/2024/04/Cerebral-Palsy-Clinical-Practice-Guideline.pdf
References
Davis DW. Review of cerebral palsy, Part I: Description, incidence, and etiology. Neonatal Netw. 1997 Apr;16(3):7-12. PMID: 9155357.
Davis DW. Review of cerebral palsy, Part II: Identification and intervention. Neonatal Netw. 1997 Jun;16(4):19-25; quiz 26-9. PMID: 9216317.
Dove, D. et al. Developmental disabilities issues exploration forum: Cerebral palsy. Agency for Healthcare Research and Quality. AHRQ Publication No. 11(12)-EHC078-EF October 2011
Huang L, Zhang C, Gu J, Wu W, Shen Z, Zhou X, Lu H. A randomized, placebo-controlled trial of human umbilical cord blood mesenchymal stem cell infusion for children with cerebral palsy. Cell Transplant. 2018 Feb;27(2):325-334. doi: 10.1177/0963689717729379. PMID: 29637820; PMCID: PMC5898688.
Jones MW, Morgan E, Shelton JE, Thorogood C. Cerebral palsy: introduction and diagnosis (part I). J Pediatr Health Care. 2007 May-Jun;21(3):146-52. doi: 10.1016/j.pedhc.2006.06.007. PMID: 17478303.
Krach LE. Pharmacotherapy of spasticity: oral medications and intrathecal baclofen. J Child Neurol. 2001 Jan;16(1):31-6. doi: 10.1177/088307380101600106. PMID: 11225954.
Krigger KW. Cerebral palsy: an overview. Am Fam Physician. 2006 Jan 1;73(1):91-100. PMID: 16417071.
Matthews DJ, Balaban B. Beyin felçli çocuklarda spastisitenin tedavisi [Management of spasticity in children with cerebral palsy]. Acta Orthop Traumatol Turc. 2009 Mar-Apr;43(2):81-6. Turkish. doi: 10.3944/AOTT.2009.081. PMID: 19448346.
Mathewson MA, Lieber RL. Pathophysiology of muscle contractures in cerebral palsy. Phys Med Rehabil Clin N Am. 2015 Feb;26(1):57-67. doi: 10.1016/j.pmr.2014.09.005. PMID: 25479779; PMCID: PMC4258234.
Naletilić M, Tomić V, Sabić M, Vlak T. Cerebral palsy: early diagnosis, intervention and risk factors. Coll Antropol. 2009 Dec;33 Suppl 2:59-65. PMID: 20120401.
Novak I, Morgan C, Fahey M, Finch-Edmondson M, Galea C, Hines A, Langdon K, Namara MM, Paton MC, Popat H, Shore B, Khamis A, Stanton E, Finemore OP, Tricks A, Te Velde A, Dark L, Morton N, Badawi N. State of the evidence traffic lights 2019: Systematic review of interventions for preventing and treating children with cerebral palsy. Curr Neurol Neurosci Rep. 2020 Feb 21;20(2):3. doi: 10.1007/s11910-020-1022-z. PMID: 32086598; PMCID: PMC7035308.
Raina P, O’Donnell M, Rosenbaum P, Brehaut J, Walter SD, Russell D, Swinton M, Zhu B, Wood E. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. 2005 Jun;115(6):e626-36. doi: 10.1542/peds.2004-1689. PMID: 15930188.
Tilton AH. Therapeutic interventions for tone abnormalities in cerebral palsy. NeuroRx. 2006 Apr;3(2):217-24. doi: 10.1016/j.nurx.2006.01.008. PMID: 16554259; PMCID: PMC3593441.
Vitrikas K, Dalton H, Breish D. Cerebral palsy: An overview. Am Fam Physician. 2020 Feb 15;101(4):213-220. PMID: 32053326.
Wimalasundera N, Stevenson VL. Cerebral palsy. Pract Neurol. 2016 Jun;16(3):184-94. doi: 10.1136/practneurol-2015-001184. Epub 2016 Feb 2. PMID: 26837375.

