Spinal Tumors
A tumor occurs when cells overproduce tissue leading to a mass or swelling. It is an abnormal growth of tissue. A tumor should not be confused with a cyst which is a sac filled with air, fluid, pus, or other material. This overproduction of cells or damaged cells can occur anywhere in the body including the spinal cord and/or brain.
Tumors develop because of mutations (genetic changes) in the DNA tissue within cells. This allows the affected tissue to grow faster than normal. The area of fast growth becomes a tumor. Causes of tumor development can be from gene mutations, inherited conditions, family histories of cancer, exposure to toxins including smoking and benzine among others, radiation exposure, excessive sunlight exposure, obesity, and viruses.
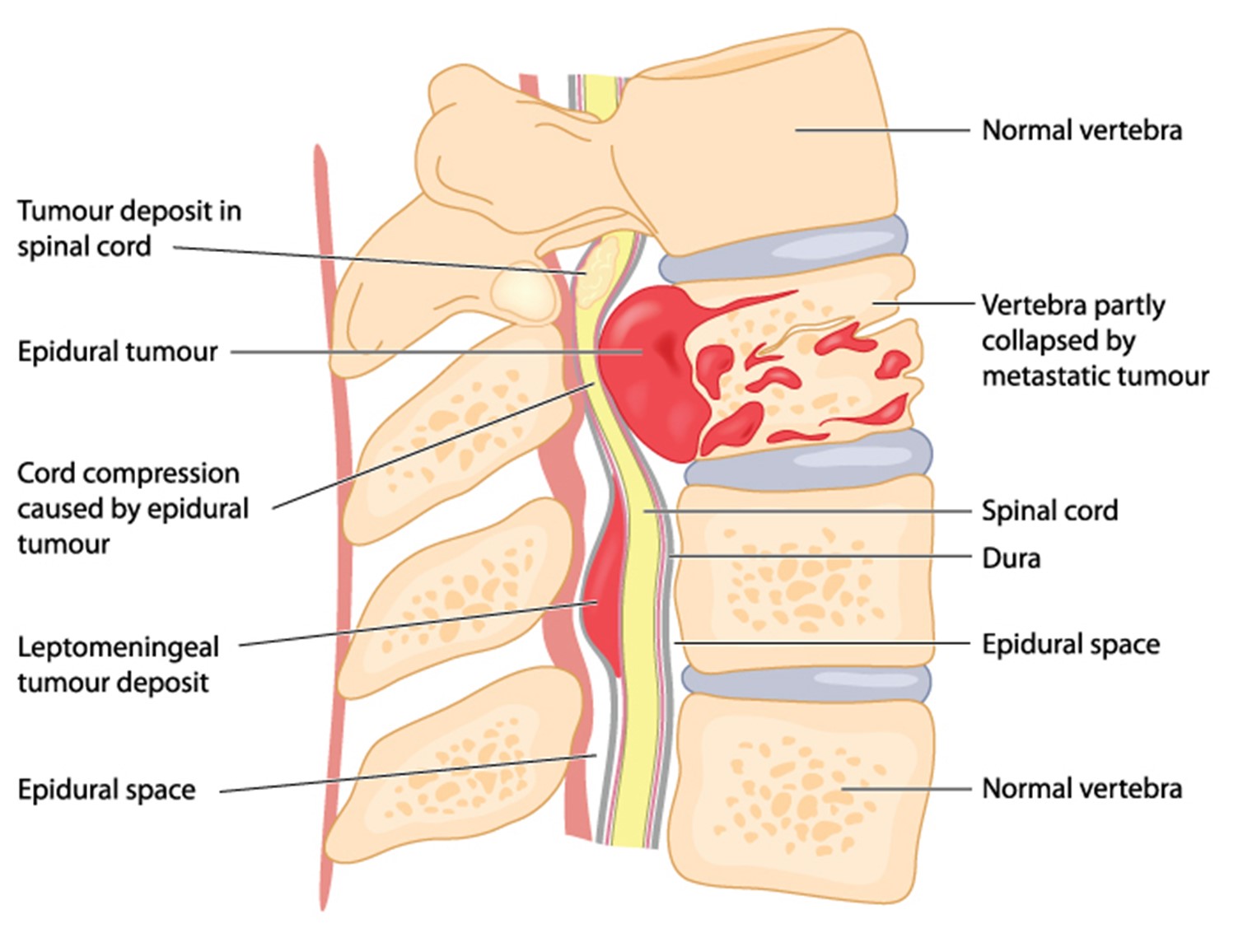
In the spine, tumors develop within the spinal cord (intramedullary), next to the spinal cord but still within the protective spinal membrane called the dura (intradural-extramedullary), or outside the surrounding dura (extramedullary). Tumors can also develop in the bones of the vertebrae which can lead to pressure in the spinal canal.
The image below represents the location of spinal cord tumors within the vertebrae and spinal cord.
Some tumors are benign (not cancerous) and others are spreadable (metastatic). Those that are spreadable cancer can begin in the spine and spread to other parts of the body or start in other parts of the body and spread to the spine.
The term primary tumors indicates that the tumor developed at the site of the tumor location (it did not travel through the body from another location). Most are often not cancerous however some primary tumors are malignant or can evolve to malignancy.
There are three different classifications of primary tumors. These include:
- Primary spinal tumors that begin within the spinal column. They are most often benign, which means they are not cancerous and do not spread throughout the body. They are usually non-life threatening and may or may not require surgical removal.
- Premalignant tumors are just starting to develop. They may become life-threatening if left untreated.
- Malignant tumors are cancerous which can be life-threatening. These can spread to nearby tissue and organs as well as throughout the body. Some return even after treatment.
Secondary Tumors are cancerous. These are called secondary tumors because affected cells have traveled from some other location in the body. However, secondary tumors can also arise at the site of origin.
- Metastasis from primary cancer is the collective name for any tumor in or around the spinal cord that has spread to other parts of the body or a tumor in another part of the body that has spread to the spinal cord.
- Secondary primary cancer is a different type of cancer that develops in another part of the body. It is two separate types of cancer in one person.
Types of spinal tumors are named for the location in the spine where the tumor developed.
These tumors are generally not cancerous:
Aneurysmal bone cysts are fast-growing blood-filled tumors inside the bone usually in the knee, pelvis or spine. These tumors damage the bone and surrounding tissue. Because of their quick growth treatment is required.
Eosinophilic granuloma occurs when the body overproduces immune cells creating hardened growths. This usually occurs in boys between the age of five to 10 years from an extremely rare disease called Langerhans cell histiocytosis.
Giant cell tumor is an aggressive tumor that occurs mostly in the extremities, knee, wrist or shoulder but occasionally in the sacrum or lumbar area of the spine. Surgery and medication are offered for treatment. The exact cause is unknown but thought to be from trauma, environmental issues or diet.
Hemangioblastoma is a benign tumor in the cells of the lining of the blood vessels in the spinal cord, brain or retina. Due to the limited space by the vertebrae, there is no room for extra pockets of blood. The bundle of blood presses against and collapses delicate spinal cord tissue which leads to sensation and functional issues in the body depending on the location of the hemangioblastoma’s location or locations.
Meningioma develops from the meninges or protective lining of the brain and spinal cord. Meningioma is most often not cancerous but very rarely can be malignant. They can appear anywhere in the meninges of the brain or spinal cord but most often appear in the thoracic region (rib cage area). They can lead to loss of sensation, function and partial paralysis. Meningiomas can grow into surrounding tissue.
Nerve sheath tumor occurs in the insulation layer of a nerve called myelin and the connective tissue that surrounds it. They can occur as one tumor or several. These tumors include schwannomas and neurofibromas among others.
- Schwannoma is a tumor that begins in the lining of the spinal nerve cells called myelin. Because myelinated nerve cells are in the lower spine, pain and decreased sensation and function occurs in the legs.
- Neurofibromas are tumors that grow from nerve cells. The condition is most often genetically inherited but can occur spontaneously in very rare cases. When diagnosed, the condition is called Neurofibromatosis.
Osteoid osteoma are small tumors that occur singly or multiply from osteoblasts and osteoclasts which are components of the bone. It can lead to scoliosis. Most often these develop in males between the age of 4-25 however, there are rare cases in females.
Spinal hemangioma are benign tumors in the mid and lower back. They typically have no to few symptoms and appear in individuals between the ages of 30-50 years. If symptomatic, they affect sensory and motor function.
Spinal neurofibroma are tumors of the nerve sheath. They do occur but are rarely seen within the spinal cord. More often they are in the peripheral nervous system (nerves outside of the brain and spinal cord) which allows them to interrupt individual nerves of the nerve bundles. If many tumors appear, the diagnosis of neurofibromatosis is made. In the body, they are slow growing and do not cause symptoms. Within the spinal cord, they can place pressure on the nerves of the central nervous system.
Spinal osteoblastoma starts from an overproduction of osteoblasts which are a normal component in bones. This tumor can develop anywhere in the body but mostly occurs in the spine, hands or feet. Typically, it is found in adolescents and young adults.
Spinal osteochondroma is a rare, slow growing tumor most often in the growth plate in the bone of the C2 vertebra in the spine. It develops in childhood but stops growing when the skeletal system matures.
Vascular Malformation can occur anywhere in the body, even in the spinal cord or brain. Blood vessels can overgrow becoming tangled which creates pockets of extra blood that cannot be accommodated by the vertebrae or can rupture allowing blood to flow into the spinal column or spinal cord compressing the nerve tissue.
These tumors are cancerous and can be metastatic (spread to other parts of the body):
Chordoma is a cancer of the bone that can occur anywhere in the spine but mostly lumbar or thoracic level of the spine. It can also develop in the base of the skull. There are three types:
- Classic/conventional chordoma is the most common, often appearing at the base of the skull. The unique feature of this tumor is cells that look bubbly.
- Dedifferentiated chordoma is a mix of abnormal cells, faster growing, more aggressive and more likely to metastasize.
- Poorly differentiated chordoma is caused from a deletion in the gene SMARCB1 or INI1. It is found in children and young adults. Only sixty cases have been reported.
Ewing’s sarcoma is a bone and soft tissue cancer occurring in children and young adults. This cancer is not inherited but develops from spontaneous changes in the genes EWSR1 chromosome 22 and FLI1. It changes the genetic makeup of the individual.
Glioma develops in the brain or spinal cord from the supportive and protective cells of nerves.
- Astrocytoma is a type of tumor developed from genetic IDH-mutants of multiple varieties. These tumors have no border between the tumor and normal central nervous system tissue.
- Ependymoma starts in the brain or spinal cord from an overgrowth of glial cells. Types include:
- Subependymoma develop near the ventricles in the brain, more often found in adults
- Myxopapillary ependymoma develops in the lower spinal cord most often in adult men
- Classic ependymoma is the most common type of an overgrowth of glia cells
- Anaplastic ependymoma develops in the brain base and spreads
- Oligodendroglioma is a tumor of oligodendrocyte cells which creates the substance that protect nerves. It is a single tumor that has defined borders with swelling around the tumor.
- Glioblastoma arises from genetic mutations from IDH-wildtype in that there are two copies of the IDH gene. The cells of this tumor develop from astrocytes (balance biochemical function of in the brain) of the glial cells, multiply quickly and can spread to other parts of the body.
Metastases of organ cancers Cancer that develops in other parts of the body can spread to the brain and spine. This is called metastasis. At times, treatment to the tumor in the brain or spine must be treated. In other cases, treating the source of cancer along with treatment of areas where the cancer has spread is necessary.
Multiple Myeloma is cancer of the blood cells, particularly white blood cells, in the body. Since blood flows to every part of the body, unhealthy plasma cells spread this cancer to all areas especially the bones. This can lead to bone fractures especially in the vertebrae of the spine where the bones collapse leading to pressure on the spinal cord.
Symptoms
Just as the brain is held within the rigid bones of the skull, the spinal cord is located within the bony vertebrae in the back from the brain to the tailbone. The bony vertebrae do not allow for expansion therefore, there is only room for the spinal cord, blood, and spinal fluid. There is not any room for anything else such as internal bleeding or extra cell growth such as a tumor because the bone cannot expand. Therefore, any extra tissue such as a tumor will press on the delicate tissue of the spinal cord leading to functional impairment and sometimes paralysis and pain.
Symptoms of a tumor in the spine depend on the type of tumor, your general health, and the location.
Type of tumor: Primary tumors are those that arise within the spinal cord or supporting structures. These tumors usually slowly progress. Secondary tumors are those that have spread from other parts of the body or metastasize. These tumors progress quickly.
Your general health: If you have paralysis from any condition or trauma, you may not sense pain or loss of function due to a tumor.
Location of tumor: The location of a tumor can affect the symptoms. If the tumor is within the spinal cord, within the dura surrounding the spinal cord, outside the dura, or in bone, the progression of symptoms will vary. Symptoms of tumors within or surrounding the spinal cord usually are noted sooner as opposed to tumors outside of the dura of the spinal cord since the dura might protect the spinal cord from pressure for a short time.
The location of the spinal tumor will affect functions at that level. Symptoms may expand to above and below the tumor level, vary by tumor location and size, and may not appear evenly on both sides of the body.
Symptoms of a spinal tumor may appear singly, or with multiple issues. Usually, symptoms develop over time, however some develop symptoms suddenly. Rarely will anyone have all these symptoms. The most common symptoms include:
- Pain ranging form intermittent aches from coughing or straining, to severe, continuous pain
- Breathing difficulty ranging from shortness of breath to apnea
- Swallowing difficulty, choking
- Muscle tone or spasms that can range from twitches to cramps
- Muscle weakness leading to stumbles, falls, dropping things
- Muscle stiffness especially in the neck or back
- Reflexes may be slow to absent
- Sensations that are decreased or changed such as numbness or tingling noted in parts of the body
- Walking changes
- Bladder and/or bowel control decreased or lost
- Scoliosis or curvature of the spine
- Paralysis or paratheses
- Headaches, nausea, and vision issues can occur especially in tumors located higher in the spinal cord
This diagram depicts the body function responsibilities at each level of the spinal cord.

Diagnosis
Diagnosis of a spinal tumor may include some or all the following:
History and Physical Examination is performed to assess your general state of health and to note changes in your usual function. Be sure to report any changes in your body function and sensation as well as when symptoms began.
Neurological Examination is conducted to assess your nervous system function including sensation, function, weakness, and reflexes. Tenderness and pain will be assessed.
Blood Tests provide information about your general health but will also indicate the type of cancer that may be present. They can indicate if the tumor is primary or if it has metastasized from another part of the body. Some examples of blood tests include CBC (complete blood count), blood protein tests, circulating tumor cell tests, and tests of DNA for genetic links.
Urine Tests may be requested to ensure internal organs are functioning such as the liver and kidneys to ensure spinal tumor treatments can be tolerated.
Genetic Testing may be performed to assess the DNA of the tumor and to monitor family traits.
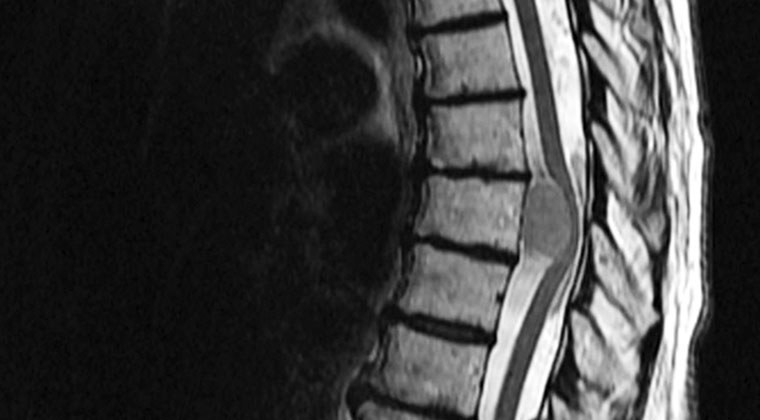
Imaging Tests may vary depending on the certainty of diagnosis. For example, an X-ray may be done to see if there is any gross problem in the spine. More definitive imaging including CT scan (computerized tomography uses computer driven radiology to define the image) or MRI (magnetic resonance imaging, assesses tissue composition) will be used to pinpoint the location of the tumor and what structures are affected. PET scans (Positive Emission Tomography) include a radiographic dye injected through an IV to assess organ and tissue functions.
Bone Scan can locate abnormal areas in your spinal vertebrae as well as in the other bones of your body. This can help locate the area or areas of tumor.
Lumbar Punction (Spinal Tap) may be performed to assess if tumor cells are in the cerebral spinal fluid and to assess if the tumor has spread.
Biopsy is a procedure where a needle is inserted to remove tumor tissue. For spine tumors this is done under anesthesia, using MRI or CT scans to guide the approach with either a needle or through an incision.
Tumor Markers are biological factors within your body that have been identified for some types of cancer. These may be monitored through laboratory studies of your blood, saliva, urine, stool, bone marrow, or from within the tumor. They can indicate the presence of cancer, an assessment of your treatment effectiveness, recovery, or recurrence. Tumor markers are also used for evaluation of individuals who require particular medications that may result in cancer. If the markers change, the medication plan is altered so you do not develop cancer.
Treatments
How tumors of the spine are treated vary depending on the location, size, source and type of tumor.
Primary tumors that are not metastatic or cancerous may not require treatment. If a primary tumor is causing health issues such as pain or pressing on the nerves of the spinal cord leading to changes in function, surgery may be required for removal.
Secondary tumors that have metastasized from other parts of the body that are of one type of cancer are treated with a plan for treatment of that type of cancer throughout the body. For instance, breast, prostate, and lymph node cancers are some of the types of cancer that travel throughout the body. Treatment is for the cause of the tumor as opposed to just treating the tumor in the spine.
Treatment plans are based on the needs of the individual. The protocols are based on extensive research to provide the most effective and appropriate treatment. Some individuals will have just one type of treatment listed below; others will have combinations of treatments.
Chemotherapy is medication that can be provided in several forms such as pill, injection, or infusion. This is given on a schedule where treatment occurs over time. The treatment dose, form of medication, and schedule are determined by your specific need. Chemotherapy may be used prior to surgery to shrink the tumor, after therapy to help eradicate traces of the tumor from the body, or as a stand-alone treatment. Supplemental medication is provided to help control side effects of chemotherapy.
Radiation therapy is the use of radiation beams (energy) to destroy cancer cells, stop division of cancer cells, or to shrink the size of a tumor by the destruction of the tumor’s genetic material reducing or eliminating the tumor’s ability to reproduce and survive. This treatment is given outside of the body by a highly controlled beam to the cancer cells while avoiding healthy cells, or by an implant placed inside the body in or near the tumor (brachytherapy).
Immunotherapy is a nonsurgical treatment that stimulates the immune system to attack the cancer cells. This treatment can be delivered in several ways including by injection to interrupt the genetic material of the cancer cells.
Surgery may be performed if the spinal tumor is resistant to chemotherapy or radiation and in a location where the tumor can be safely removed. It may be open surgery or minimally invasive. Bone cement is used to repair the vertebrae after the tumor is removed.
Stereotactic Radiosurgery is a procedure where high-dose radiation is delivered from outside of the body to the tumor. Individually, the tiny beams of radiation do not destroy healthy tissue but when they cross at the location of the tumor, the tumor tissue is destroyed. Surgery or making an incision into the body is not done. Patients go home after the procedure is completed. There can be side effects such as pain at the tumor site, skin changes, nausea, vomiting and diarrhea. There are several types of stereotactic radiosurgery including Gamma Knife, stereotactic body radiation therapy, proton therapy, and linear accelerator.
After the treatment plan is completed, your medical team will determine follow up procedures to monitor your health and to assess if further treatment will be required over time.
Rehabilitation or Therapies
Primary care provider may be a general practitioner, family medicine practitioner, or nurse practitioner who you routinely see for healthcare. This medical professional may be the first person you see for symptoms that are diagnosed as a spinal tumor. They will follow your care through the treatment of the tumor and will continue with your general health care.
A neurologist is a specialist in the care of the nervous system. You may already be under the care of a neurologist for your health issues. They will perform tests to diagnose a spinal tumor, direct you to a specialist spinal surgeon or oncologist (cancer specialist), and provide follow-up care after treatment.
Spinal surgeon and Vascular surgeon may become involved if the treatment plan involves surgery. You may see both or either of these specialists. The spinal surgeon is a neurosurgeon with a specialty in spinal surgery. If the tumor involves the blood system, a vascular surgeon who operates on blood vessels may be involved or may be the surgeon for your needs.
Medical Oncologist is a cancer treatment specialist that provides the plan and treatment of chemotherapy. They may work in conjunction with a radiation specialist, and surgeon, if that is a part of your plan.
Radiation Oncologist provides the plan and treatment of radiation therapy.
Orthopedic, urological, and other medical providers will be involved with your health treatment as needed.
Physiatrist is a rehabilitation specialist that may be required if you have lingering issues with recovery. This physician will provide rehabilitation treatments and strategies to help you recover and gain strength in affected areas.
Rehabilitation Registered Nurses can assist you with self-care practices, especially bladder and bowel issues to help restore or control continence.
Physical and Occupational Therapists can provide treatments for mobility, self-care, continence issues and equipment that will aid in your recovery or adaptations.
Psychiatrist, Psychologist or Mental Health Professionals can assist you and your family with strategies for dealing with life-threatening or life-altering diagnoses and treatments.
History
As summarized from the American Cancer Society website (https://www.cancer.org/cancer/understanding-cancer/history-of-cancer.html):
Cancer was first recorded in Egyptian writings 3,000 years ago.
Hippocrates was the first to describe and name cancer.
Visualization of cancer cells was not possible until the development of the microscope in the 1800s.
Once cancer was understood, treatments began to be developed.
The importance of cancer screening to diagnose and treat cancer early was emphasized in the 1900s.
For treatment of brain and spinal tumors, often the location of a tumor is difficult to surgically reach due to the delicate tissue of the nervous system. In 1949, stereotactic radiosurgery was developed by Lars Leksell so tumors within the central nervous system could be removed without injuring the surrounding nervous system. This technique continues to be refined.
Today, the treatment of spinal tumors continues to be studied including advancements in genetic research and gene manipulation treatments. New protocols for treatment of specific types of cancer are being researched to improve outcomes and therapeutic treatments.
Research is also being conducted to improve chemotherapy treatments in the central nervous system to overcome the blood-spinal cord barrier.
Facts and Figures
Primary spinal tumors are rare.
The ages of onset of primary tumors are most often between 10 and 16 years old and 65 and 74 years old.
Benign (non-cancerous) primary spinal tumors occur in 0.5% of all diagnosed tumors. Malignant or cancerous primary spinal tumors occur less often.
Secondary spinal tumors or those that have developed from metastasis occur in 97% of all cases.
Resources
If you are looking for more information on brain and spinal tumors or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 7:00 am to12:00 am (midnight) EST.
Additionally, the Reeve Foundation maintains a brain and spinal tumors fact sheet with additional resources from trusted Reeve Foundation sources. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
We encourage you to reach out to organizations, including associations which feature news, research support, and resources, national networks of support groups, clinics, and specialty hospitals.
Community Resources:
American Cancer Society https://www.cancer.org/
Clinical Guidelines:
Spinal Cord Injury:
Paralyzed Veterans of America: https://pva.org
CNS Cancer:
Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, Hawkins C, Ng HK, Pfister SM, Reifenberger G, Soffietti R, von Deimling A, Ellison DW. The 2021 WHO Classification of Tumors of the Central Nervous System: A Summary. Neuro Oncol. 2021 Aug 2;23(8):1231-1251. doi: 10.1093/neuonc/noab106. PMID: 34185076; PMCID: PMC8328013.
Nabors LB, Portnow J, Ahluwalia M, Baehring J, Brem H, Brem S, Butowski N, Campian JL, Clark SW, Fabiano AJ, Forsyth P, Hattangadi-Gluth J, Holdhoff M, Horbinski C, Junck L, Kaley T, Kumthekar P, Loeffler JS, Mrugala MM, Nagpal S, Pandey M, Parney I, Peters K, Puduvalli VK, Robins I, Rockhill J, Rusthoven C, Shonka N, Shrieve DC, Swinnen LJ, Weiss S, Wen PY, Willmarth NE, Bergman MA, Darlow SD. Central Nervous System Cancers, Version 3.2020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2020 Nov 2;18(11):1537-1570. doi: 10.6004/jnccn.2020.0052. PMID: 33152694.
Redjal N, Venteicher AS, Dang D, Sloan A, Kessler RA, Baron RR, Hadjipanayis CG, Chen CC, Ziu M, Olson JJ, Nahed BV. Guidelines in the Management of CNS Tumors. J Neurooncol. 2021 Feb;151(3):345-359. doi: 10.1007/s11060-020-03530-8. Epub 2021 Feb 21. PMID: 33611702.
Neurosurgery:
Horbinski C, Nabors LB, Portnow J, Baehring J, Bhatia A, Bloch O, Brem S, Butowski N, Cannon DM, Chao S, Chheda MG, Fabiano AJ, Forsyth P, Gigilio P, Hattangadi-Gluth J, Holdhoff M, Junck L, Kaley T, Merrell R, Mrugala MM, Nagpal S, Nedzi LA, Nevel K, Nghiemphu PL, Parney I, Patel TR, Peters K, Puduvalli VK, Rockhill J, Rusthoven C, Shonka N, Swinnen LJ, Weiss S, Wen PY, Willmarth NE, Bergman MA, Darlow S. NCCN Guidelines® Insights: Central Nervous System Cancers, Version 2.2022. J Natl Compr Canc Netw. 2023 Jan;21(1):12-20. doi: 10.6004/jnccn.2023.0002. PMID: 36634606.
Radiology:
Cox BW, Spratt DE, Lovelock M, Bilsky MH, Lis E, Ryu S, Sheehan J, Gerszten PC, Chang E, Gibbs I, Soltys S, Sahgal A, Deasy J, Flickinger J, Quader M, Mindea S, Yamada Y. International Spine Radiosurgery Consortium Consensus Guidelines for Target Volume Definition in Spinal Stereotactic Radiosurgery. Int J Radiat Oncol Biol Phys. 2012 Aug 1;83(5):e597-605. doi: 10.1016/j.ijrobp.2012.03.009. Epub 2012 May 19. PMID: 22608954.
Redmond KJ, Robertson S, Lo SS, Soltys SG, Ryu S, McNutt T, Chao ST, Yamada Y, Ghia A, Chang EL, Sheehan J, Sahgal A. Consensus Contouring Guidelines for Postoperative Stereotactic Body Radiation Therapy for Metastatic Solid Tumor Malignancies to the Spine. Int J Radiat Oncol Biol Phys. 2017 Jan 1;97(1):64-74. doi: 10.1016/j.ijrobp.2016.09.014. Epub 2016 Sep 17. PMID: 27843035; PMCID: PMC5600487.
Pain:
The American Cancer Society:
Aman MM, Mahmoud A, Deer T, Sayed D, Hagedorn JM, Brogan SE, Singh V, Gulati A, Strand N, Weisbein J, Goree JH, Xing F, Valimahomed A, Pak DJ, El Helou A, Ghosh P, Shah K, Patel V, Escobar A, Schmidt K, Shah J, Varshney V, Rosenberg W, Narang S. The American Society of Pain and Neuroscience (ASPN) Best Practices and Guidelines for the Interventional Management of Cancer-Associated Pain. J Pain Res. 2021 Jul 16;14:2139-2164. doi: 10.2147/JPR.S315585. PMID: 34295184; PMCID: PMC8292624.
References
Ahlhelm FJ, Fries P, Nabhan A, Reith W. Spinale Tumoren [Spinal Tumors]. Radiologe. 2010 Feb;50(2):165-78; quiz 179-80. German. doi: 10.1007/s00117-009-1841-z. PMID: 19669725.
Alektoroff K, Papanagiotou P. Spinale Tumoren im Kindesalter [Pediatric Spinal Tumors]. Radiologie (Heidelb). 2023 Aug;63(8):609-613. German. doi: 10.1007/s00117-023-01178-9. Epub 2023 Jul 5. PMID: 37407746.
Avila MJ, Walter CM, Skoch J, Abbasifard S, Patel AS, Sattarov K, Baaj AA. Fusion After Intradural Spine Tumor Resection in Adults: A Review of Evidence and Practices. Clin Neurol Neurosurg. 2015 Nov;138:169-73. doi: 10.1016/j.clineuro.2015.08.020. Epub 2015 Aug 28. PMID: 26355808.
Bădilă AE, Rădulescu DM, Niculescu AG, Grumezescu AM, Rădulescu M, Rădulescu AR. Recent Advances in the Treatment of Bone Metastases and Primary Bone Tumors: An Up-to-Date Review. Cancers (Basel). 2021 Aug 23;13(16):4229. doi: 10.3390/cancers13164229. PMID: 34439383; PMCID: PMC8392383.
Barbagallo GMV, Maione M, Raudino G, Certo F. Thoracic Intradural-Extramedullary Epidermoid Tumor: The Relevance for Resection of Classic Subarachnoid Space Microsurgical Anatomy in Modern Spinal Surgery. Technical Note and Review of the Literature. World Neurosurg. 2017 Dec;108:54-61. doi: 10.1016/j.wneu.2017.08.078. Epub 2017 Aug 24. PMID: 28843754.
Bludau F, Reis T, Schneider F, Clausen S, Wenz F, Obertacke U. Kyphoplastie kombiniert mit intraoperativer Radiotherapie (Kypho-IORT). Therapiealternative für den oligometastasierten Patienten mit Wirbelsäulenmetastasen [Kyphoplasty Combined with Intraoperative Radiotherapy (Kypho-IORT). Alternative Therapy for Patients with Oligometastatic Spinal Metastases]. Radiologe. 2015 Oct;55(10):859-67. German. doi: 10.1007/s00117-015-0018-1. PMID: 26420600.
Challapalli A, Aziz S, Khoo V, Kumar A, Olson R, Ashford RU, Gabbar OA, Rai B, Bahl A. Spine and Non-spine Bone Metastases – Current Controversies and Future Direction. Clin Oncol (R Coll Radiol). 2020 Nov;32(11):728-744. doi: 10.1016/j.clon.2020.07.010. Epub 2020 Aug 1. PMID: 32747153.
Chung AS, Chang K, Liu JC. Minimally Invasive Intradural Tumor Resection. World Neurosurg. 2021 Jan;145:243. doi: 10.1016/j.wneu.2020.09.129. Epub 2020 Sep 28. PMID: 32992063.
Costăchescu B, Niculescu AG, Iliescu BF, Dabija MG, Grumezescu AM, Rotariu D. Current and Emerging Approaches for Spine Tumor Treatment. Int J Mol Sci. 2022 Dec 10;23(24):15680. doi: 10.3390/ijms232415680. PMID: 36555324; PMCID: PMC9779730.
Csaszar N, Ganju A, Mirnics ZS, Varga PP. Psychosocial Issues in the Cancer Patient. Spine (Phila Pa 1976). 2009 Oct 15;34(22 Suppl):S26-30. doi: 10.1097/BRS.0b013e3181b95c55. PMID: 19829274.
Donthineni R. Diagnosis and Staging of Spine Tumors. Orthop Clin North Am. 2009 Jan;40(1):1-7, v. doi: 10.1016/j.ocl.2008.10.001. PMID: 19064051.
Elsamadicy AA, Koo AB, Reeves BC, Freedman IG, Pennington Z, David WB, Ehresman J, Hengartner A, Laurans M, Kolb L, Shin JH, Sciubba DM. Cost and Health Care Resource Utilization Differences After Spine Surgery for Bony Spine versus Primary Intradural Spine Tumors. World Neurosurg. 2021 Jul;151:e286-e298. doi: 10.1016/j.wneu.2021.04.015. Epub 2021 Apr 15. PMID: 33866030.
Epstein FJ, Farmer JP. Pediatric Spinal Cord Tumor Surgery. Neurosurg Clin N Am. 1990 Jul;1(3):569-90. PMID: 2136159.
Gao X, Li L, Cao J, Zhao Y, Liu Y, Yang J, Dong L, Wan W, Liu T, Xiao J. Symptomatic Postoperative Spinal Epidural Hematoma After Spine Tumor Surgery: Incidence, Clinical Features, and Risk Factors. Spinal Cord. 2019 Aug;57(8):708-713. doi: 10.1038/s41393-019-0281-5. Epub 2019 Apr 17. PMID: 30996340.
Garg S, Dormans JP. Tumors and Tumor-Like Conditions of the Spine in Children. J Am Acad Orthop Surg. 2005 Oct;13(6):372-81. doi: 10.5435/00124635-200510000-00002. PMID: 16224110.
Hersh AM, Lubelski D, Theodore N, Sciubba DM, Jallo G, Shimony N. Approaches to Incidental Intradural Tumors of the Spine in the Pediatric Population. Pediatr Neurosurg. 2023;58(5):367-378. doi: 10.1159/000530286. Epub 2023 Mar 22. PMID: 36948181.
Hsu W, Jallo GI. Pediatric Spinal Tumors. Handb Clin Neurol. 2013;112:959-65. doi: 10.1016/B978-0-444-52910-7.00016-7. PMID: 23622304.
Massaad E, Ha Y, Shankar GM, Shin JH. Clinical Prediction Modeling in Intramedullary Spinal Tumor Surgery. Acta Neurochir Suppl. 2022;134:333-339. doi: 10.1007/978-3-030-85292-4_37. PMID: 34862557.
Morito S, Yamada K, Nakae I, Sato K, Yokosuka K, Yoshida T, Shimazaki T, Hazemoto Y, Saruwatari R, Nishida K, Okazaki S, Hiraoka K. Intradural Extramedullary Tumor Location in the Axial View Affects the Alert Timing of Intraoperative Neurophysiologic Monitoring. J Clin Monit Comput. 2023 Jun;37(3):775-782. doi: 10.1007/s10877-022-00971-6. Epub 2023 Jan 13. PMID: 36635568.
Niznick N, Nguyen TB, Bourque PR. Spinal Capillary Hemangioma: A Rare Benign Extradural Tumor. Can J Neurol Sci. 2020 Jul;47(4):549-550. doi: 10.1017/cjn.2020.60. Epub 2020 Mar 26. PMID: 32213223.
Noh T, Vogt MS, Pruitt DW, Hummel TR, Mangano FT. Pediatric Intramedullary Spinal Cord Tumor Outcomes Using the WeeFIM Scale. Childs Nerv Syst. 2018 Sep;34(9):1753-1758. doi: 10.1007/s00381-018-3831-9. Epub 2018 May 25. PMID: 29797065.
Noureldine MHA, Shimony N, Jallo GI. Malignant Spinal Tumors. Adv Exp Med Biol. 2023;1405:565-581. doi: 10.1007/978-3-031-23705-8_22. PMID: 37452954.
Noureldine MHA, Shimony N, Jallo GI. Benign Spinal Tumors. Adv Exp Med Biol. 2023;1405:583-606. doi: 10.1007/978-3-031-23705-8_23. PMID: 37452955.
Ogawa BK, Skaggs DL, Kay RM. Malignant Peripheral Nerve Sheath Tumor of the Lumbar Spine. Am J Orthop (Belle Mead NJ). 2009 May;38(5):E89-92. PMID: 19585001.
Ottenhausen M, Ntoulias G, Bodhinayake I, Ruppert FH, Schreiber S, Förschler A, Boockvar JA, Jödicke A. Intradural Spinal Tumors in Adults-Update on Management and Outcome. Neurosurg Rev. 2019 Jun;42(2):371-388. doi: 10.1007/s10143-018-0957-x. Epub 2018 Feb 17. PMID: 29455369.
Puac-Polanco P, Guarnizo A, Cruz JP, Rodriguez FR, Torres CH. Intradural Extramedullary Tumors and Associated Syndromes. Neuroimaging Clin N Am. 2023 Aug;33(3):407-422. doi: 10.1016/j.nic.2023.03.002. Epub 2023 Apr 25. PMID: 37356859.
Quiceno E, Hussein A, Pico A, Abdulla E, Bauer IL, Nosova K, Moniakis A, Khan MA, Farhadi DS, Prim M, Baaj A. Indications for Fusion with Intradural Spine Tumor Resection in Adults: A Systematic Review and Meta-Analysis. World Neurosurg. 2023 Aug;176:21-30. doi: 10.1016/j.wneu.2023.04.041. Epub 2023 Apr 18. PMID: 37080455.
Tekkök IH. Intramedullary Epidermoid Cysts. J Neurosurg Spine. 2008 Feb;8(2):202-3; author reply 203. doi: 10.3171/SPI/2008/8/2/202. PMID: 18248296.
Tokuhashi Y, Ajiro Y, Oshima M. Algorithms and Planning in Metastatic Spine Tumors. Orthop Clin North Am. 2009 Jan;40(1):37-46, v-vi. doi: 10.1016/j.ocl.2008.09.002. PMID: 19064054.
Yáñez ML, Miller JJ, Batchelor TT. Diagnosis and Treatment of Epidural Metastases. Cancer. 2017 Apr 1;123(7):1106-1114. doi: 10.1002/cncr.30521. Epub 2016 Dec 27. PMID: 28026861.
Yoon SH, Kim KJ, Chung SK, Kim HJ, Choe G, Chung SB, Jin YJ. Inflammatory Myofibroblastic Tumor in the Intradural Extramedullary Space of the Lumbar Spine with Spondylolisthesis: Case Report and Peview of the Literature. Eur Spine J. 2010 Jul;19 Suppl 2(Suppl 2):S153-7. doi: 10.1007/s00586-009-1212-5. Epub 2009 Nov 26. PMID: 19941012; PMCID: PMC2899620.
Zheng GB, Hong Z, Wang Z. Diagnostic Value of MRI in Coexistence of Schwannoma and Meningioma Mimicking a Single Dumbbell-Shaped Tumor in High Cervical Level. Case Series and Literature Review. J Spinal Cord Med. 2023 Mar;46(2):326-331. doi: 10.1080/10790268.2021.1977062. Epub 2021 Oct 6. PMID: 34612798; PMCID: PMC9987764.

