Deep Vein Thrombosis
Blood flows easily through all the arteries and veins in your body as the heart circulates it. However, if blood collects in a vein, a blood clot is formed. This narrows or even blocks the blood vessels from allowing blood to flow through smoothly. Venous thromboembolism occurs when blood clots in a small vein close to the skin’s surface. When a blood clot forms in a vein deeper in the body, it is diagnosed as Deep Vein Thrombosis (DVT). DVT prevents the efficient flow of blood and can dislodge traveling through the body which leads to life-threatening conditions. This can occur in one area or several areas at one time.
Blood clots can be helpful such as when the skin is cut. The scab is a dry blood clot that stops blood from flowing out of the body and prevents infection in the inner body. The scab will protect the wound until the body inside the skin has healed. However, when a blood clot occurs within the body, circulation is disrupted.
Blood clots in your arteries are created from plaque. The arteries have higher pressure within them compared to veins. The high artery pressure sends blood to your major organs and all body parts. Pressure in your artery is measured when your blood pressure is assessed. Too much pressure in the arteries is high blood pressure. Plaque in the arteries creates atherosclerosis (decreased elasticity of arteries) which leads to hypertension, cardiac/vascular issues, and neurological issues including stroke.
Veins have a lower pressure. A blockage or clot in the vein slows the blood from returning to the heart. The blockage typically occurs around a valve in the vein. The clot creates a little ‘dam’ within the vein making blood back up in the blood vessel. The pooling blood enlarges the clot. The vein behind the clot can swell from blood that cannot get through at the rate it should be traveling. This can be painful if you have sensation in that part of your body.
The term, deep vein thrombosis, is used because blood clots are formed in veins deep within the body. The deep veins are usually next to bones. They mostly appear in the legs, arms, and groin. Typically, just one side of the body is affected. DVT in the leg can occur in the deep veins including the popliteal vein (behind the knee), femoral vein (in the thigh), common femoral vein (in the thigh from knee to groin), or iliac veins (in the pelvis). In the groin, DVT occurs in the femoral vein. In the arm, DVT can occur in the brachial vein (upper arm), axillary (armpit), and subclavian veins (below the collar bone) and also in the radial (forearm), ulnar (forearm), and internal jugular (neck) veins.
A DVT can travel throughout the body if it detaches from the vein wall. A DVT that travels to the lungs is called a pulmonary embolism which affects your ability to breathe. This can lead to severe complications including death.
Some common risk factors for developing DVT include:
- Immobility from lack of movement
- Injury from an accident or health condition
- Paget-Schroetter Syndrome (PSS) (overuse or repetitive motions in the arms)
- Extra body weight
- Constricting blood flow (crossing legs, hooking arm on the back of the wheelchair, compression stockings wrinkled or rolled down tops, tight clothing)
- Improper wheelchair fit (especially pressure on the back of the knee)
- Too tight leg bag straps (especially as the leg bag fills)
- Improper fit of braces and splints on legs or arms
- Broken bone or muscle injury
- Infection
- Varicose veins
- Major surgery
- Over the age of 40
- Previous DVT or family history of DVT
- Heart disease, lung disease, inflammatory bowel disease, kidney disease
- Smoking
- Inherited or other blood coagulation conditions such as thrombophilia
- Central line catheter
- Pacemaker or defibrillator
- Pregnancy and in the three months after delivery
- Some birth control pills or replacement hormones
- Cancer or cancer treatment
Symptoms/Diagnosis
The symptoms of DVT vary. Many individuals have no symptoms at all. If you have issues with sensation, you may have symptoms that are not felt. Therefore, it is important to look at your body, including using a mirror to see areas that cannot be viewed directly. Many DVTs are not noted in 30-40% of cases due to variability of symptoms.
Pain occurs from the blood flow backing up behind the clot which stretches the vein or due to the clot pressing on the vein. Some DVTs cause pain, while others do not. If sensation is present, you may or may not feel pain. This can be throbbing, or sharp pains, or both. Pain may increase if standing, walking, or with exercise. If sensation is present, pain can increase when pushing the toes toward your knee or moving the arms.
Swelling occurs from the pooling of blood below the DVT. Veins may appear swollen and hard or sore. The hard vein may be felt with a light touch. A DVT may be present if one arm or leg has more swelling than the other. Edema generally occurs in both extremities in spinal cord injury but can also appear in one extremity with head injury, stroke, or other neurological issues. Note the amount of edema you normally have so you will be able to determine if it becomes greater which may indicate a DVT.
Warmth An area of DVT will often feel warmer than the surrounding skin. Gently placing your hand over the tender or suspected area, will provide a general feeling of increased skin temperature over a DVT. Sometimes no temperature change is present.
Skin Pigment Changes in the shape of a streak can occur with DVT. Skin pigment changes are more common in venous thromboembolism (VTE) than in DVT. Darkly pigmented skin may have a purplish hue over the area of DVT. Lightly pigmented skin might look pinkish. Sometimes a pigment change streak begins at the location of the blockage and continues below.
Fever can occur with DVT. It is generally low grade, not extremely elevated.
Autonomic Dysreflexia episodes can occur if the DVT is below the level of injury. DVT is a noxious stimulation to the body. AD is a response that something is wrong in the body below the level of injury. If other DVT symptoms are present with an unexplained episode(s) of AD, or an increase in AD symptoms, DVT should be suspected. More information about AD symptoms and treatment can be found here: https://www.ChristopherReeve.org/cards
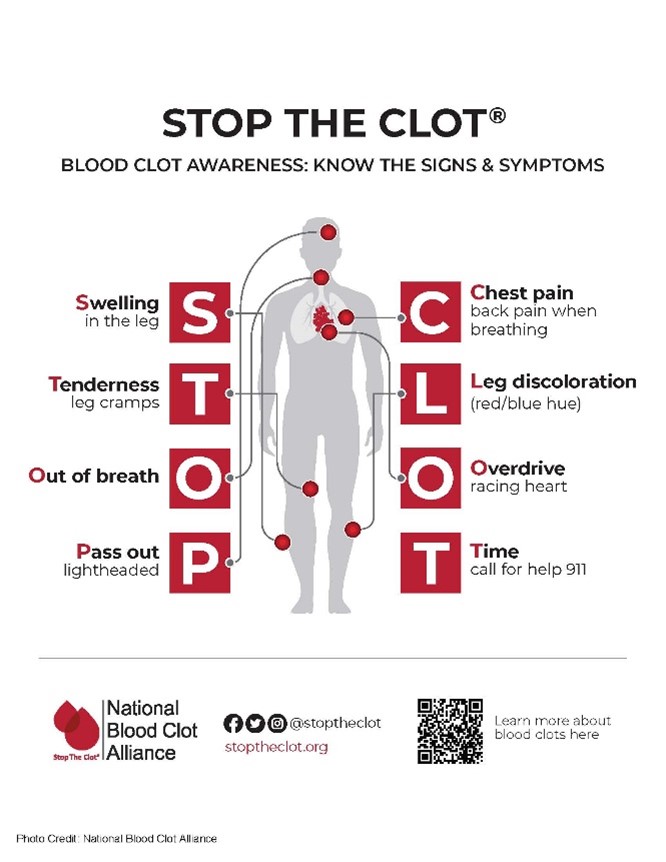
An Embolus occurs when a DVT breaks away from the vein and travels through the body, especially to the lungs. This is a medical emergency. Respiratory emergency symptoms of a traveling DVT include trouble breathing, low blood pressure, fainting, increased heart rate, chest discomfort/pain, coughing with or without blood, or episodes of AD. If DVT progresses to the lungs, pain may be felt on inhalation (breathing in), shortness of breath can occur, or blood may be coughed up.
The image below is a depiction of DVT in the leg. Symptoms anywhere in the body may not be this subtle.

Diagnosing a DVT begins with a review of your symptoms. Reporting when the issue started, and all your symptoms and self-treatments is critical to diagnosis.
A list of all medications is necessary including prescribed, over-the-counter, and recreational medications as these can affect your treatment plan.
A complete medical examination is performed including a history of illnesses and surgeries.
A duplex ultrasound is the usual test for DVT. It is conducted over your body in the area of the suspected clot. This non-invasive test consists of a gel and wand placed on top of the skin. Sound waves create an image of the inside of the vein which will show the presence or absence of a clot. For individuals with some healthcare needs, the duplex ultrasound is replaced with contrast venography where contrast dye is injected into the suspected area.
A blood test will be done to assess the presence of a substance called D-dimer. High levels of D-dimer indicate the presence of a blood clot. A negative D-dimer indicates no blood clot.
On rare occasions, a CT scan or MRI will be done to see if a blood clot is present in the body. Typically, this is only done to check for DVT if other health issues are present.
The Christopher & Dana Reeve Foundation has developed a downloadable wallet card to assist you with understanding DVT symptoms and tips for talking with healthcare professionals about symptoms and treatment. All Foundation wallet cards are available in multiple languages. https://www.ChristopherReeve.org/cards
Diagnosing Pulmonary Embolus
DVTs produce a risk of pulmonary embolus (PE) or a DVT that travels to the lungs. These tests are only performed if a PE is suspected.
Computed Tomographic Pulmonary Angiography (CTPA) is a specialized CT scan of the lungs. This is the main test procedure used to assess the occurrence of pulmonary embolus. The DVT is suspected to have been released into the bloodstream and traveled through the body to the lungs.
Ventilation-perfusion (V/Q) scan is an alternative to CTPA. This assesses oxygenation and blood flow in the lungs using a contrast dye.
Pulmonary angiography is a procedure that uses a contrast dye to show images of blood vessels in the lungs. Due to the invasiveness of this assessment, it is only used as an alternative test to those listed above.
MRI may be used to diagnose pulmonary embolus in patients allergic to contrast dye or those who are pregnant.
Treatments
Individuals with DVT are prescribed compression garments that may include leg stockings, arm sleeves, and abdominal binders. Chest compression garments may also be ordered as needed. These are medical-grade garments, not over-the-counter, to ensure the correct amount of pressure is applied.
Anticoagulation is the most common treatment of DVT. It is given either by IV or oral medication.
Anticoagulants, taken either by injection or orally. are the main treatment for DVT. These medications reduce the blood’s ability to clot. This medication may be used to dissolve and reabsorb an existing clot. Anticoagulants also help in the long-term prevention of further blood clot development.
Injectable anticoagulants include the following among others:
- Unfractionated heparin is given through an IV in the hospital but also might be used at home in some cases. This quick-acting drug activates antithrombin making clots more difficult to form while allowing the body to dissolve an existing DVT. Monitoring of the drug in your blood is required through regular blood tests for partial thromboplastin time (PTT), a blood test that assesses how long it takes for your blood to clot. Separately from DVT, this medication is injected into an IV lock to prevent a blood clot at that site. Brand names include:
- Calcilean
- Hepalean
- Liquaemin
- Novaheparin
- Low molecular weight heparin is injected under the skin typically in the abdomen. It also makes clots more difficult to form while allowing the body to dissolve an existing DVT. The duration of this drug is longer so less frequent blood tests are required. This medication is routinely provided to individuals in the hospital who have had a major injury or have immobility. It also can be given at home. Brand names include:
- Dalteparin
- Enoxaparin (Lovenox)
- Tinzaparin
- Fondaparinux is injected under the skin typically in the abdomen. Its purpose is to reduce clotting in the blood. The formulation is different from heparin. Brand names include:
- Arixtra
Oral medications for DVT include the following among others:
- Anticoagulants:
- Dabigatran(Pradaxa)
- Warfarin (Jantoven)
- IX inhibitors (dissolve blood clots with less risk of bleeding)
- Apixaban (Eliquis)
- Edoxaban (Lixiana, Savaysa)
- Rivaroxaban (Xarelto)
Over-the-Counter Medication may be prescribed when your treatment of anticoagulants or IX medications has been completed. This is typically long-term treatment. Aspirin is the drug of choice which may be given as one 325 mg adult tablet or baby aspirin at 81mg. Do not begin an aspirin regimen without discussing it with your healthcare provider.
Thrombolytic Agents are used if clots need to be more quickly dissolved than the body’s natural rate for dissolving. This medication is delivered by a catheter placed in your vein threaded to the clot site. Drugs used to dissolve the clot are:
- Alteplase (Activase)
- Anistreplase (Eminase)
- Reteplase (Retavase)
- Tenecteplase (Metalyse, TNKase)
ALERT: If you have a diagnosed DVT or other blood clot, it is imperative that you follow instructions for taking your medication and follow-up blood tests.
- Keep up with the required blood work as the effects of blood thinning medication can quickly become too much or too little.
- Testing to monitor your blood clotting time will allow time to adjust your medication dosage as needed.
- Read the package instructions as some foods can interfere with these medications.
- Monitor for bleeding from your body. For example, a small cut may bleed excessively requiring a pressure dressing, or you may notice blood in your urine or stool. Alert your healthcare provider if any bleeding issues occur.
If antithrombotic or thrombolytic agents are not successfully treating your DVT or if they are not recommended due to other health conditions, medical procedures may be used. These are more invasive treatments.
An inferior vena cava filter (IVC) is a small device placed in the main vein in your lower body using interventional radiology (use of X-ray-guided insertion). Some are temporarily placed while others are permanent. Once the device is placed, it is opened like an umbrella to catch small clots before they can travel to more dangerous locations. It is used to prevent a DVT from becoming a PE, however, it may also be used in the case of the presence of a DVT complicated by medical conditions that can lead to bleeding in other parts of the body, if blood thinners do not work, or with other serious medical conditions.
In some cases, surgery can be necessary to remove the blood clot. Rarely the clot might dislodge or break off a part during the procedure. Also, additional clots can form due to the procedure.
Prevention of DVT
Avoiding the development of a DVT is the best treatment. Sometimes a DVT still forms but using preventive measures will reduce your risk.
Compression leg stockings, arm sleeves, chest, and abdominal binders can increase the tone in your extremities and abdomen. The compression helps facilitate blood return flow to the heart, especially with immobility and paralysis. Be sure they are smooth, not rolled at one end, or wrinkled as this creates constriction pressure within your body. In the hospital, intermittent leg compression pumps are used. This device applies intermittent pressure to the legs to help avoid DVT. Rarely, some individuals will use these at home as well.
Avoid pressure areas, especially under the arms and behind the knees. Keep elastic stockings and sleeves smooth without creasing at joints. Avoid ‘hooking’ your arm on the back of your wheelchair or the back of your knees pressing against your seat. Do not cross your legs or ankles as the pressure can impede blood flow.
Monitor the tightness of equipment straps and clothing. Check the tightness of orthotics. A leg bag strap may be loose when applied to the leg but will become tighter as the bag fills or with dependent leg edema. Tight clothes that constrict your body under the arm, inner elbow, groin, behind the knees, or at the ankles can restrict blood flow.
Be kind to your body when moving your legs and arms. Do not throw your body around but gently move yourself or have yourself gently moved.
Be safety conscious by avoiding situations that could result in falls, feet falling off footrests, arms falling off armrests, or fingers getting caught in wheels. Be cautious on uneven surfaces when walking or wheeling.
Stay active by moving all the parts of your body, including areas with less mobility. If you cannot exercise your body by moving your legs with your hands, have someone assist you. Perform pressure releases to help maintain your skin and circulation.
Check your skin for pressure injury and signs of deep vein thrombosis development.
Avoid deep massages that can release an unknown blood clot.
Eat healthfully avoiding salty items that increase blood pressure, keep your cholesterol in normal ranges, and, if needed reduce your weight which adds pressure to the veins in your lower body.
Stay hydrated within restrictions of bladder management or cardiac programs.
Quit smoking which increases your risk of blood clots or adds to the risk of having other blood clots.
Women, check with your healthcare professional for the birth control or hormone replacement therapy that best fits your needs.
Rehabilitation or Therapies
Medication may be needed for a limited period or a lifetime. Compression garments will be used for two years after DVT or longer.
These professionals will assist you in recovery:
A primary care physician or your regular healthcare professional will most likely diagnose and monitor care for DVT. They will continue to monitor you long-term to avoid DVT recurrence and medication levels.
A vascular specialist typically will provide more diagnostic assessments and treatments for the active period of the DVT. You may see them after your DVT has resolved to help avoid a recurrence.
A hematologist specializes in blood issues. They may be consulted if you have medical concerns with blood clotting.
Physical and occupational therapists will help you with exercise and mobility issues after the DVT has resolved or slowly return you to your base level of function. They can also provide safety information (making you and your home safe), equipment that can assist in putting on compression garments, and exercises to keep you healthy.
History
The first recorded case of DVT was in 1271. This report was about a 20-year-old cobbler named Raoul who developed a DVT in his right leg. During the Renaissance period, DVT was treated as most other health issues with bloodletting. It was in 1872 that the German surgeon, Trendelenburg noticed sudden mortality associated with pulmonary embolism. During early history, most DVTs were associated only with pregnancy.
With the development of the birth control pill, it was noted that more women developed complications, especially DVT. Currently, the formulation of contraceptives and hormone replacement medication has been improved, making the DVT risk far less.
In the 1940s oral anticoagulants became available. This led the way to more thrombolytic therapies and faster rates of dissolving blood clots. Today, the standard of care is anticoagulant therapy. Due to these advancements, there is less hospitalization and more use of anticoagulant treatment at home.
Facts and Figures
The American Heart Association notes that 1.2 million individuals in the United States are affected by DVT. Being over the age of 40 years increases risk.
Death from DVT and PE is estimated to be 300,000 per year making it the third most common vascular disease.
Males are slightly more prone to developing DVT.
March is bleeding disorders awareness month.
A white ribbon with a red stripe represents Deep Vein Thrombosis awareness and treatment.
Download a Life-Saving DVT Wallet Card
One of the folds is written specifically for the physician. In the event of a DVT crisis, you can pull the “Attention Physician” flap to the front. This allows first responders to see your personal information on one side, and directions to treat DVT on the other.
The DVT card applies to both adults and children. Copies of the DVT card are available online for download, or you can call the National Paralysis Resource Center directly at 800-539-7309 and ask to speak to our Information Specialists.
Watch Our Video on DVT
Resources
For more information on understanding DVT and additional resources from trusted Reeve Foundation sources, please download our fact sheet on deep vein thrombosis. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
The information contained in the wallet card and web page is presented to inform you about paralysis and its effects. Nothing contained herein is to be construed or intended as a medical diagnosis or treatment. Contact your physician or other qualified healthcare provider should you have questions on your health, treatment, or diagnosis.
We encourage you to reach out to organizations, including associations that feature news, research support, resources, national networks of support groups, clinics, and specialty hospitals.
Clinical Guidelines
Ortel TL, Neumann I, Ageno W, Beyth R, Clark NP, Cuker A, Hutten BA, Jaff MR, Manja V, Schulman S, Thurston C, Vedantham S, Verhamme P, Witt DM, D Florez I, Izcovich A, Nieuwlaat R, Ross S, J Schünemann H, Wiercioch W, Zhang Y, Zhang Y. American Society of Hematology 2020 Guidelines for Management of Venous Thromboembolism: Treatment of Deep Vein Thrombosis and Pulmonary Embolism. Blood Adv. 2020 Oct 13;4(19):4693-4738. doi: 10.1182/bloodadvances.2020001830. PMID: 33007077; PMCID: PMC7556153.
Alexopoulou-Prounia L, Kakkos SK, Gohel M. European and US Guidelines on Acute DVT Management. J Cardiovasc Surg (Torino). 2024 Feb;65(1):5-11. doi: 10.23736/S0021-9509.23.12861-8. Epub 2024 Feb 1. PMID: 38300165.
University of Arkansas for Medical Sciences. Deep Vein Thrombosis Guidelines in Spinal Cord Injury. 2020. https://medicine.uams.edu/pmr/wp-content/uploads/sites/3/2021/02/Guidelines-SCI-Deep-Vein-Thrombosis-2020.pdf
Agency for Healthcare Research and Quality. Your Guide to Preventing and Treating Blood Clots: https://www.ahrq.gov/patients-consumers/prevention/disease/bloodclots.html
Community Resources
American Heart Association: https://www.heart.org/
National Blood Clot Alliance: https://www.stoptheclot.org/learn_more/signs-and-symptoms-of-blood-clots/
References
Ageno W, Haas S, Weitz JI, Goldhaber SZ, Turpie AGG, Goto S, Angchaisuksiri P, Dalsgaard Nielsen J, Kayani G, Farjat AE, Zaghdoun A, Schellong S, Bounameaux H, Mantovani LG, Prandoni P, Darius H, Kakkar AK. Upper Extremity DVT versus Lower Extremity DVT: Perspectives from the GARFIELD-VTE Registry. Thromb Haemost. 2019 Aug;119(8):1365-1372. doi: 10.1055/s-0039-1688828. Epub 2019 Jun 10. PMID: 31183844.
Altobelli MG, Quinonez RA. When Should DVT Be Suspected in Children with Osteomyelitis? Hosp Pediatr. 2012 Jul;2(3):167-72. doi: 10.1542/hpeds.2012-0011. PMID: 24319921.
Anderson FA, Audet AM. Physician Practices in the Prevention of Deep Vein Thrombosis: The Masspro DVT Study. Orthopedics. 1996 Aug 2;19:9. doi: 10.3928/0147-7447-19960802-04. PMID: 24826701.
Badireddy M, Mudipalli VR. Deep Venous Thrombosis Prophylaxis. 2023 May 7. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30521286.
Barrosse-Antle ME, Patel KH, Kramer JA, Baston CM. Point-of-Care Ultrasound for Bedside Diagnosis of Lower Extremity DVT. Chest. 2021 Nov;160(5):1853-1863. doi: 10.1016/j.chest.2021.07.010. Epub 2021 Jul 13. PMID: 34270964.
Boon GJAM, Van Dam LF, Klok FA, Huisman MV. Management and Treatment of Deep Vein Thrombosis in Special Populations. Expert Rev Hematol. 2018 Sep;11(9):685-695. doi: 10.1080/17474086.2018.1502082. Epub 2018 Jul 25. PMID: 30016119.
Citla Sridhar D, Abou-Ismail MY, Ahuja SP. Central Venous Catheter-Related Thrombosis in Children and Adults. Thromb Res. 2020 Mar;187:103-112. doi: 10.1016/j.thromres.2020.01.017. Epub 2020 Jan 15. PMID: 31981840.
Davidson BL. DVT Treatment in 2000: State of the Art. Orthopedics. 2000 Jun;23(6 Suppl):s651-4. PMID: 10875431.
Denny N, Musale S, Edlin H, Serracino-Inglott F, Thachil J. Chronic Deep Vein Thrombosis. Acute Med. 2018;17(3):144-147. PMID: 30129947.
Diana Yap FS, Ng ZY, Wong CY, Muhamad Saifuzzaman MK, Yang LB. Appropriateness of Deep Vein Thrombosis (DVT) Prophylaxis Use Among Medical Inpatients: A DVT Risk Alert Tool (DRAT) Study. Med J Malaysia. 2019 Feb;74(1):45-50. PMID: 30846662.
Duffett L. Deep Venous Thrombosis. Ann Intern Med. 2022 Sep;175(9):ITC129-ITC144. doi: 10.7326/AITC202209200. Epub 2022 Sep 13. PMID: 36095313.
Goldhaber SZ, Magnuson EA, Chinnakondepalli KM, Cohen DJ, Vedantham S. Catheter-Directed Thrombolysis for Deep Vein Thrombosis: 2021 Update. Vasc Med. 2021 Dec;26(6):662-669. doi: 10.1177/1358863X211042930. Epub 2021 Oct 4. PMID: 34606385; PMCID: PMC9009765.
Goshgarian C, Gorelick PB. DVT Prevention in Stroke. Curr Neurol Neurosci Rep. 2017 Sep 18;17(10):81. doi: 10.1007/s11910-017-0782-6. PMID: 28921057.
Jenkins JS, Michael P. Deep Venous Thrombosis: An Interventionalist’s Approach. Ochsner J. 2014 Winter;14(4):633-40. PMID: 25598728; PMCID: PMC4295740.
Khan O, Marmaro A, Cohen DA. A Review of Upper Extremity Deep Vein Thrombosis. Postgrad Med. 2021 Aug;133(sup1):3-10. doi: 10.1080/00325481.2021.1892390. Epub 2021 Mar 8. PMID: 33618595.
Kahn SR. The Post-Thrombotic Syndrome. Hematology Am Soc Hematol Educ Program. 2016 Dec 2;2016(1):413-418. doi: 10.1182/asheducation-2016.1.413. PMID: 27913509; PMCID: PMC6142466.
Kakkos S, Kirkilesis G, Caprini JA, Geroulakos G, Nicolaides A, Stansby G, Reddy DJ. Combined Intermittent Pneumatic Leg Compression and Pharmacological Prophylaxis for Prevention of Venous Thromboembolism. Cochrane Database Syst Rev. 2022 Jan 28;1(1):CD005258. doi: 10.1002/14651858.CD005258.pub4. PMID: 35089599; PMCID: PMC8796751.
Lin S, Alepuz A, Tritsch T, Schwartz G. Deep Vein Thrombosis Prophylaxis in Orthopedic Surgery. Cureus. 2024 Feb 6;16(2):e53726. doi: 10.7759/cureus.53726. PMID: 38455781; PMCID: PMC10919879.
Lockner D, Paul C, Hedlund B, Schulman S, Nyman D. Thermography in the Diagnosis of DVT. Thromb Haemost. 1981 Oct;46(3):652-4. PMID: 7314058.
Lv B, Wang H, Zhang Z, Li W. Distribution Characteristics of Perioperative Deep Vein Thrombosis (DVT) and Risk Factors of Postoperative DVT Exacerbation in Patients with Thoracolumbar Fractures Caused by High-Energy Injuries. Eur J Trauma Emerg Surg. 2024 Feb 28. doi: 10.1007/s00068-024-02468-0. Epub ahead of print. PMID: 38416184.
Modi S, Deisler R, Gozel K, Reicks P, Irwin E, Brunsvold M, Banton K, Beilman GJ. Wells Criteria for DVT is a Reliable Clinical Tool to Assess the Risk of Deep Venous Thrombosis in Trauma Patients. World J Emerg Surg. 2016 Jun 8;11:24. doi: 10.1186/s13017-016-0078-1. PMID: 27279896; PMCID: PMC4898382.
Muñoz Rodríguez FJ. Diagnosis of Deep Vein Thrombosis. Rev Clin Esp. 2020 Jun 27:S0014-2565(20)30132-6. English, Spanish. doi: 10.1016/j.rce.2020.03.009. Epub ahead of print. PMID: 32600570.
Paydar S, Sabetian G, Khalili H, Fallahi J, Tahami M, Ziaian B, Abbasi HR, Bolandparvaz S, Ghaffarpasand F, Ghahramani Z. Management of Deep Vein Thrombosis (DVT) Prophylaxis in Trauma Patients. Bull Emerg Trauma. 2016 Jan;4(1):1-7. PMID: 27162921; PMCID: PMC4779464.
Roy M, Rajamanickam V, Chen H, Sippel R. Is DVT Prophylaxis Necessary for Thyroidectomy and Parathyroidectomy? Surgery. 2010 Dec;148(6):1163-8; discussion 1168-9. doi: 10.1016/j.surg.2010.09.013. PMID: 21134547.
Sachdeva A, Dalton M, Lees T. Graduated Compression Stockings for Prevention of Deep Vein Thrombosis. Cochrane Database Syst Rev. 2018 Nov 3;11(11):CD001484. doi: 10.1002/14651858.CD001484.pub4. PMID: 30390397; PMCID: PMC6477662.
Shaikhouni A, Baum J, Lonser RR. Deep Vein Thrombosis Prophylaxis in the Neurosurgical Patient. Neurosurg Clin N Am. 2018 Oct;29(4):567-574. doi: 10.1016/j.nec.2018.06.010. PMID: 30223969.
Sforza M, Husein R, Saghir R, Saghir N, Okhiria R, Okhiria T, Sidhu M, Zaccheddu R. Deep Vein Thrombosis (DVT) and Abdominoplasty: A Holistic 8-Point Protocol-Based Approach to Prevent DVT. Aesthet Surg J. 2021 Sep 14;41(10):NP1310-NP1320. doi: 10.1093/asj/sjab011. PMID: 33450008.
Tamura S, Yamamoto M, Kitagawa A, Nagao T. Deep Vein Thrombosis (DVT) Prophylactic Team Activity to Support DVT Prevention Protocol for the Purpose of the Prophylaxis of Pulmonary Thromboembolism (PTE) and Operation. Ann Vasc Dis. 2021 Jun 25;14(2):99-107. doi: 10.3400/avd.oa.21-00017. PMID: 34239633; PMCID: PMC8241545.
Turkoski B. Preventing DVT in Orthopaedic Patients. Orthop Nurs. 2000 May-Jun;19(3):93-9. doi: 10.1097/00006416-200019030-00014. PMID: 11153340.
Wang X, Jiang Z, Li Y, Gao K, Gao Y, He X, Zhou H, Zheng W. Prevalence of Preoperative Deep Venous Thrombosis (DVT) Following Elderly Intertrochanteric Fractures and Development of a Risk Prediction Model. BMC Musculoskelet Disord. 2022 May 4;23(1):417. doi: 10.1186/s12891-022-05381-y. PMID: 35509097; PMCID: PMC9065244.
Wang L, Ma X, Chen Y, Gao S, Pan W, Chen J, Su L, He H, Long Y, Yin C, Zhou X; China National Critical Care Quality Control Centre Group (China-NCCQC). Factors Influencing DVT Formation in Sepsis. Thromb J. 2024 Jan 16;22(1):11. doi: 10.1186/s12959-024-00582-y. PMID: 38229151; PMCID: PMC10790559.
Zhang Y, Xia H, Wang Y, Chen L, Li S, Hussein IA, Wu Y, Shang Y, Yao S, Du R. The Rate of Missed Diagnosis of Lower-Limb DVT by Ultrasound Amounts to 50% or so in Patients Without Symptoms of DVT: A Meta-Analysis. Medicine (Baltimore). 2019 Sep;98(37):e17103. doi: 10.1097/MD.0000000000017103. Erratum in: Medicine (Baltimore). 2019 Dec;98(49):e18469. doi: 10.1097/MD.0000000000018469. PMID: 31517841; PMCID: PMC6750306.