Sexual Health for Men
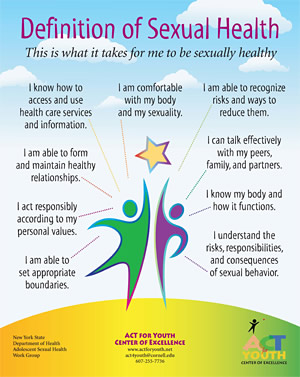
Sexual health and sexuality are among the concerns of individuals with nervous system issues including spinal cord injury, brain injury, and neurological diseases. This is a normal part of life and should be considered a part of your rehabilitation program. Sexuality is an expression of yourself. It includes your feelings toward other individuals as well as yourself. Sexual health focuses on your sexual well-being as well as the reproductive system. It consists of ‘physical, mental, and social well-being in relation to sexuality and requires a positive and respectful approach to sexuality, sexual relationships, as well as pleasurable and safe sexual experiences’ (World Health Organization).
The desire to share a sexual experience with someone you find attractive physically, emotionally, and sexually is a fundamental part of life. Because of changes after neurological disease or trauma, you may find your sexuality is intact but there is a difference in how your body responds. Navigating these changes can be daunting as finding resources to guide you through adaptations can be challenging. However, a positive body image and satisfying sex life are absolutely possible for everyone.
Sexual experiences often begin with relationships. Meeting, courting, and getting to know another individual can be the elements of a strong relationship. Finding comfort in your abilities and your partner can help build a successful and satisfying sexual relationship.
Although male/female terminology is being used, it is for distinguishing the mechanics of body functions, not individual sexual identity. Your sexuality is your own.
Sexual Violence
Sexual violence is an issue that can affect anyone. Being in a relationship includes the safety of your physical body as well as your mental health. Maintenance of your personal integrity is a part of sexual health. If you are uncomfortable in a relationship, for any reason, reconsider it. Individuals who feel less positive about themselves or their abilities may accept unhealthy relationships because they feel unworthy or unattractive to others. This is not a reason to accept a partner. Everyone has the right to be treated respectfully and have your wishes considered. This includes all relationships both sexual and non-sexual. If you feel you are being mistreated, call the RAINN (Rape, Abuse and Incest National Network) National Sexual Assault Hotline at 800-656-4673. Staff members can help you sort through your concern, even if sexual abuse has not yet occurred. They will connect you with resources in your community.
Children
Early in life, children will explore their bodies including genitalia. It is not for sexual stimulation, but as a way to learn about their own bodies. They may learn that there are body differences between boys and girls. Usually, they will notice differences at potty training or bath time if with other siblings. Children with neurological injury may not know about gender body differences when catheterized or during a bowel program when an adult does the caregiving. As the child transitions into their ability to self-care for their toileting needs, these differences may be noted. However, in the child’s world, they will assume their toileting process is standard practice.
It is important for a child to learn about appropriate adult behavior when assisting with bladder and bowel issues. Transitioning to self-care for toileting is important to development and maturity.
Children with neurological issues prior to the onset of puberty can be at risk for issues with body development. Brain injury can lead to hormonal development issues. Spinal cord injury prior to puberty very often leads to scoliosis or underdeveloped legs. Monitor these concerns with your healthcare professional.
Puberty
Puberty is a developmental stage of life when an individual’s body develops sexual maturity. In males, it starts most typically between the ages of 12 and 16. Hormones involved with sexual development in males include androgens–one of which is testosterone.
Due to hormonal changes, the penis and testicles increase in overall size, hair develops in the armpits and groin, and eventually, on the face, muscles develop, and the voice deepens. This is a time when acne becomes an issue. There is a significant growth spurt, especially in height. Males may develop a slight increase in breast tissue. Emotional changes can be a challenge to manage.
The onset of puberty can be earlier, before age nine, and is called precocious puberty. This can happen for a variety of reasons. One is relying on tube feeding formula for nutrition as it can provide hyper nutrition and calories. Lack of movement of the body can also be a reason for early puberty due to decreased energy expenditure.
Delayed puberty in males is defined as no testicle development by age 14 or incomplete testicle and penis development five years after the onset of puberty. Reasons for delayed puberty are malnutrition which can occur from a poor diet or low-calorie intake, increased energy used by the body as with tone (spasms), or high energy expenditure with the movement for walking. A brain tumor or brain injury can disrupt hormonal production changes creating a delay in puberty.
Teens with chronic healthcare issues, including neurological injury or disease may have some issues with adjustment to puberty. They may be used to less privacy during personal care, especially with toileting, they may not have information about their sexual function unique to their physical abilities, or they may not have the opportunity for sexual exploration privately or within a relationship.
Physiology — The Body’s Sexual Responses
Both men and women have a sexual response cycle. This occurs in four phases for both genders. In men, the cycles appear with the following characteristics:
- Excitement may last from a few minutes to several hours. Some or all of these responses may be included: increased muscle tension, faster heart rate, breathing, and blood pressure, flushed skin (blotches on the face, neck, chest, back), hardness in the nipples, increased blood flow to the penis resulting in erection, swelling in the testicles, tightening scrotum, secretion of a small amount of semen from the tip of the penis.
- Plateau varies in length of time and may be controlled if the sexual response is intact. Variants in the length of time may be affected by neurological issues. Responses include increased intensity from the excitement phase, ascension of the testicles within the scrotum, increased heart rate, breathing, and blood pressure, and increased muscle intensity especially in the feet, face, and hands.
- Orgasm, sometimes called climax, occurs for seconds. In this phase, involuntary muscle contractions begin, peaks occur in heart rate, breathing, and blood pressure, increased intake of oxygen, increased tension in muscles, rhythmic contractions at the base of the penis resulting in ejaculation, and the appearance of a rash on the body. At the end of the orgasm phase, there is a forceful release of tension in the body.
- Resolution is the last phase where the body returns to its previous state. This includes the return to the individual’s normal heart rate, breathing, and blood pressure, engorgement of the genitals returns to baseline, skin flushing and color change resolves. The individual may be fatigued but has a sense of well-being. Males have a refractory period where they need recovery time before further orgasms can recur. Refractory time varies for men and can be longer with age and neurological issues.
Response to sexual situations often need to be controlled. If you are in a situation where a sexual experience is not appropriate, stopping the sexual response cycle early may be necessary. It may be critical in many situations to contain the sexual response cycle in the arousal or plateau phase for social acceptance. This can be a challenge after neurological injury if you do not have control over erectile function. Wearing less form-fitting attire may disguise a reflex erection. If you are in an agreeable sexual situation, allow the sexual response cycle to take its course.
In the brain, the hypothalamus (which controls the autonomic nervous system or ANS,) controls sex drive. The ANS controls automatic responses in the body, just one of which is the body’s response to sexual stimulation from cues from the senses. Other key areas of the brain include the subcortical (diencephalon, pituitary gland, limbic structures, and basal ganglia) and cortical (outer layer on top of the cerebrum) regions. The mesial temporal lobe and amygdala (almond-shaped mass in each cerebral hemisphere that is connected with emotions) are crucial for sex drive with the amygdala being the main structure for sexual responses. The brain controls chemicals that are released by neurotransmitters. In men, these include dopamine, oxytocin, serotonin, nitric oxide, and noradrenaline. These signaling molecules create the messages for the body’s sexual mental and physical responses.
Although these parts of the brain have specific functions, the brain works as a unit. If an area of the brain is affected by injury, stroke, or disease, that part of sexual function can be affected. For instance, if the right side of the body is affected, the left side of the body may not be able to spontaneously perform sexual functions such as movement. If the language part of the brain is affected, communication may be impaired. If the amygdala is affected, emotion control may be challenged. If there are brain effects on the neurotransmitters, the brain-body connection for sexual function can be interrupted. When the frontal lobe of the brain is affected, sexual response control may be difficult to contain.
Messages that are created in the brain and responses from the body are sent via the spinal cord. If there is an injury or disease anywhere along the spinal cord that is disrupted, messages may not be received or interpreted correctly. In particular, the pelvic plexus nerves of the somatic, thoracolumbar sympathetic, and sacral parasympathetic nerves are directly involved in genital arousal, orgasm, and ejaculation in men. A major nerve in the pelvis is the pudendal nerve that carries messages for movement and sensation of the genitalia, rectum, and bladder. The pudendal nerve exits at S2-S4. The dorsal branch of the pudendal nerve is responsible for sexual function.
Seemingly with interruptions in your brain, spinal cord, or both, sexual function may not appear to be possible, however, most individuals with neurological injury do have an active and healthy sex life, if it is desired. There are adaptations that can assist in enhancing your sexual function.
Preparation for Sex
After a neurological injury, preparation for sexual activity can make your encounter more rewarding. Knowing your body and having your partner’s understanding is important. You will have spontaneous sexual encounters with your partner but learning about how your body functions can reduce issues in the process. These tips will provide some thoughts to make the sexual encounter more successful.
Autonomic Dysreflexia (AD) is a miscommunication of messages between the brain and the body. AD is caused by something happening below your level of injury. This can be discomfort or pleasurable stimulation. Sexual stimulation can be a trigger for AD. Stimulation in the genital area, as well as sexual responses of increased blood pressure, heart rate, breathing, and flushed skin, can trigger an AD episode, which are the same as the symptoms of AD. If you have increased blood pressure, pounding headache, or other symptoms of AD, you will need to stop sexual activity. Be prepared with nitro paste or the medication that you take for AD if an AD episode appears with sexual activity. Contact your healthcare professional to provide treatment to prevent AD from recurring in your next encounter. Medication may be needed prior to sex.
Performing a bowel program before sex or on the day of a sexual encounter can eliminate the risk of bowel incontinence. A bowel accident may never occur during sex but if you are concerned, this will provide some peace of mind. As your sexual encounters increase, you will know if this is an issue for you. Most perform a bowel program prior to anal sex.
Review your bladder equipment. If you perform intermittent catheterization, you may choose to catheterize prior to sex to avoid urinary incontinence. As time passes, you will learn if you need to do this or not. If an indwelling catheter is used, you have the option of keeping it in, folding it along the side of the penis, covering it with a condom, or removing it during the sexual encounter as recommended by your healthcare professional. Suprapubic catheters should be taped to the abdomen to ensure it does not get pulled during sex. Urinary tract infections can be quite common with sexual activity in both men and women. Discuss with your health professional what is right for you.
Lubrication is essential to a sexual experience if you are considering penis-vagina, penis-rectal, or masturbation. Use a lubricant that is water-based. Oil-based lubricants leave a residue. If you have some sensation, lubricants that create a sensation of heat are helpful. If planning oral sex, some prefer flavored lubricants.
Sexually transmitted diseases are possible with or without neurological injury. Protect yourself and your partner with the use of a condom.
Contraception may be necessary even if you do not ejaculate. Seminal fluid can escape in urine which may be leaked by some.
Positioning your body can enhance your sexual experience. Use pillows, bolsters, wedges, or other positioning equipment to support your body. This can also assist with the reduction of tone (spasticity). Liberator is just one company that sells sex-oriented furniture. Gently providing range of motion to all your joints prior to sex can assist with relaxed movement and tone (spasticity). It can be a part of foreplay.
Skin care is essential during sex. Before and after sex, you will need to do pressure releases by keeping your usual turning schedule in bed or repositioning when in a chair. During sex, friction injury can occur on the skin anywhere that is rubbed such as on the back of your head, back, elbows, buttocks, thighs, and heels if your body weight is on those skin surfaces as well as on your body where your partner’s body has rubbed.
Explore your body both in areas with sensation and decreased sensation to find areas that enhance your sexual pleasure. This can include your ears, neck, nipples, areas where there are scars (scar tissue can be extremely sensitive), and erogenous zones (areas of your body that have heightened sensitivity, the stimulation of which may cause sexual arousal). This will help you find stimulation points for sexual enhancement.
Masturbation is self-stimulation. This can be used to assess what your genitals can do. If you are unsure of your erectile ability, self-stimulation can allow you to know your capabilities.
If sex will occur in your wheelchair or other mobility devices, be mindful of safety features such as tipping and falling. Be sure all brakes are locked.
Enhance the mood with gentle lighting, music, and aromas. The use of feathers, silk cloth, vibrators, or sexual toys can be added to heighten your sexual event.
Check your health and medications. Depression can affect your sexual satisfaction as well as your ability to have an erection. Diagnoses such as diabetes, obesity, and high cholesterol can affect sex as well. Alcohol, tobacco, and drug use are also culprits. Treatment of medical conditions can assist with improved sexual function.
Types of Erections
After a neurological injury, there can be effects on your ability to obtain and sustain an erection. This is due to the creation of messages to and from the brain and body. You will notice the types of erections follow upper (reflexive) and lower (areflexive) motor neuron issues in the body. These include:
Reflexogenic erection is a reflexive or spontaneous erection usually from touch or stimulation to your genitals, especially the penis. This can be from someone touching you while having sex, performing personal care, clothing rubbing, a breeze against your skin in the area, or other physical stimulation, intended or not. If you have an upper motor neuron or reflexive injury, this type of erection usually occurs. In brain injury or spinal cord injury (T10 or above), physical stimulation creates an erection reflex. Ejaculation may or may not occur.
Psychogenic erection responses are those that are created in your brain. They may include stimulation from your senses that are perceived by your brain or thoughts created in your brain. What you see, hear, touch, smell, and taste can serve as arousal stimulants. However, with brain injury, these stimulations can be misperceived or misunderstood interpretations of the actual situation. This injury coordinates with lower motor neuron injury from a brain or spinal cord injury (T11 and below). There may be some penile engorgement but not at the strength needed for sexual intercourse.
Spontaneous erections occur when your bladder is full. It is not uncommon for men to have spontaneous erections at night which are called nocturnal erections. After brain or spinal cord injury, you may still have spontaneous erections even with complete spinal cord injury and spinal cord syndromes. Intact spinal cord pathways are not necessary for spontaneous erections however, they may not be as intense as previously.
Erection Enhancement
Options exist for creating or sustaining an erection for sexual function. Discuss with your healthcare professional which is the best option for you. Always use medically approved treatments to avoid complications to your health. Individuals prefer different options depending on their life situation.
Medications Erectile dysfunction medication prescribed and advertised in the media is also used in individuals with neurological dysfunction. These medications increase reflex erections. In spinal cord injury (except cauda equina and conus medullaris, see nerve transfers below), the most effective medications are phosphodiesterase type 5 which includes sildenafil (Viagra), vardenafil (Levitra), and tadalafil (Cialis). They cannot be taken with some medications such as nitrates, some alpha-blockers, or some health issues such as retinitis pigmentosa or extreme hypotension (low blood pressure).
Intracavernosal Injections The medications of alprostadil (prostaglandin E1) or papaverine and phentolamine (B-imix or Tri-mix) is injected into the shaft of the penis to create an erection within 5 -10 minutes and lasting about an hour. Learning proper injection techniques can prevent bruising and scarring in the penis. Occasionally, priapism (a prolonged penile erection) can occur which requires medical treatment.
Intraurethral Medication Alprostadil is inserted into the urethra which creates an erection. A constriction ring can be placed at the base of the penis to maintain the erection. This treatment varies in popularity. It is used as an alternative to injections but often does not have quite the same effectiveness. The use of this technique is evolving. The constriction ring should not be in place for over 30 minutes to avoid damage to the penis.
Vacuum Device A specialized pump is placed over the penis creating increased blood flow to the penis. A ring is then placed at the base of the penis for maintaining an erection. The ring cannot be in place for over 30 minutes. These devices are available but often traded for medication treatment. Be cautious if you purchase one without medical regulation as damage to your penis can occur.
Penile Implants These implants used to be the option prior to the success of erectile medications. However, some individuals use them as an alternative. Either a silicone (somewhat flexible) prosthesis or an inflatable hydraulic prosthesis is surgically implanted into the penis. The silicone device can be placed for penetration. However, an erection is always present. It can assist with external catheter support as well. The hydraulic device has a pump implanted in the scrotum which allows for erection or relaxation of the penis. Many use the pump as an action in foreplay.
Functional Electrical Stimulation (FES) The advent of functional electrical stimulation has increased the options for erectile function. Implants can stimulate erectile function by pushing a connective button placed in the abdomen. External or transcutaneous (on the skin) devices have also offered erectile function for men.
Nerve Transfers Individuals with injury to the peripheral nerves immediately outside the spinal cord such as in cauda equina and conus medullaris may elect to have some of the peripheral nerves rerouted to create erectile potential. Other functions are not lost during this type of procedure. You will need testing with nerve conduction studies as an assessment for this treatment option.
Sexual Counseling or Sex Therapy can be used to open communication between partners as well as to create an understanding in the relationship. These services are often more far-reaching than the act of sex including ways of understanding each other and partnerships.
Testosterone Replacement Therapy may be provided if testosterone levels are low, sometimes called ‘low T’. This can assist with libido and sex drive as well as secondary sexual characteristics such as muscle building and hair loss.
Orgasm
Focusing on only penile erections as a sexual function misses the entirety of the process. In the sexual response, the brain is stimulated by the senses, seeing, hearing, touching, smelling, and tasting. More senses are being defined as well including pressure, itch, temperature, proprioception, equilibrium, and stretch receptors. Senses begin the sexual response cycle. The use of the brain and how it makes you feel sexual is essential to the process. Senses can aid in your sexual arousal process and stimulation. Many individuals use the sensations and physical expressions of their partner as a sexual enhancement. Sensing and hearing your partner’s pleasure can be used to trigger your own.
Mild vibration may enhance your erection. It can also trigger an episode of autonomic dysreflexia so be alert. Ejaculation may or may not occur. For many men with neurological injury, ejaculation may occur in to the bladder that is felt but not seen.
Orgasm can be obtained but most likely will feel different especially if your injury is complete. Those with incomplete injuries will have varied orgasm responses. An orgasm might occur with more subtle intensity. Some individuals say their orgasm feels like an overwhelming sense of calm and relaxation, others feel ‘refreshed’. The intensity and sensation of your orgasm will be unique to you. It may take several experiences to understand your response.
Fertility
Sexual activity carries a risk that can lead to pregnancy. Even if you do not ejaculate, sperm can leak. Therefore, if you are not seeking pregnancy, you or your partner should take contraceptive measures unless proven otherwise. However, for many men, fertility is an issue. Semen may be ejaculated, not ejaculated, expelled into the bladder, sperm may not have motility, meaning it may not have the capacity to travel to join an egg. Most often sperm is viable, obtaining it is more of an issue. Sperm viability and motility can be assessed in a laboratory by a healthcare professional. Performing insemination is best done for pregnancy during the woman’s ovulation cycle.
There are several ways to collect sperm:
At home:
Sexual intercourse In males who can obtain an erection with or without medication or other assistance and ejaculate out of the body from the penis, pregnancy can occur as a result of sexual intercourse.
Penile Vibrator Specially designed high-intensity vibrators are available for sperm collection. The vibrator is placed on the shaft of the penis, turned on, and semen is collected in a cup as it is released from the tip of the penis. The semen can then be immediately inserted into the female’s vagina. This device can be purchased confidentially for your personal use. It allows the creation of an intimate moment with your partner as no one else needs to be present or involved with the process. This device is used in males with spinal cord injury at T10 or above with an excellent success rate. The majority of sperm will be motile. You will want to check with your healthcare professional to ensure it is safe for you as an individual and monitor for episodes of autonomic dysreflexia (AD). For some, the risk of AD will eliminate this process as an option.
In-Home Insemination Semen can be collected in a clinical setting but insemination into the female can occur in the privacy of the home setting by the couple. Care will be needed to keep the sperm viable until the time of insemination. The healthcare professional in the clinic will provide instructions for keeping the sperm viable.
In the Clinic
Electroejaculation (EEJ) This technique can be used in all people living with spinal cord injuries. In this process, a healthcare professional inserts a probe into the rectum. An electrical current is used to stimulate ejaculation. Semen may be expelled and collected from the penis. However, if ejaculation is in to the bladder, immediate collection from the bladder is required. Lower sperm motility is noted but enough sperm can be collected for pregnancy. The process may need to be repeated over time. The procedure is usually well tolerated. It can trigger an episode of autonomic dysreflexia which requires careful monitoring during the process. The healthcare provider may encourage the partners to hold hands or occasionally for the partner to become a part of the collection process to create intimacy.
Prostatic Massage The healthcare professional massages the prostate and seminal vesicles pushing out semen through the urethra. This uses less invasive equipment but is also inconsistent in sperm collection. Episodes of autonomic dysreflexia can occur.
Surgical Sperm Retrieval (SSR) Collection of sperm through the testicle or epididymis through a surgical procedure is possible. The results of motile sperm are very low making this a low-choice option. However, there is less chance of an episode of autonomic dysreflexia.
Once semen is collected in the clinic, it may be implanted in the female using:
Intrauterine Insemination (IUI) Sperm is taken from the semen and placed directly in the female uterus. This is typically the first choice for pregnancy.
In Vitro Insemination (IVF) Fertilization of sperm and an egg, taken from a female, are fertilized in a laboratory and then implanted in a female uterus. IVF is used more with female infertility.
Intracytoplasmic Sperm Injection (ICSI) Similar to IVF, the sperm is specifically injected into an egg prior to being implanted in a female uterus. ICSI is used more with male infertility.
Other options for parenthood are adoption, fostering children, and sperm donors. These should be carefully considered based on your desire for biological children as well as taking into account your individual health concerns, religious, and cultural beliefs.
Male Cancers
Usual health checks for diseases of the male urinary and reproductive system should be conducted. This can find issues early to avoid bigger problems. Looking for lumps or changes can lead to early treatment. Sores, drainage, lumps, and color changes in the genital area is also helpful for finding cancer, sexually transmitted diseases, and rashes or pressure injury.
A testicular exam can be done in the home by the individual or their caregiver. Testicular cancer is most common in the 15-35 year age range but can appear in older men as well. Click here to find out how to perform a self-testicular exam. This is geared toward teens, but the process is the same for all men.
Prostate cancer occurs less in men with spinal cord injury than in men who do not have spinal cord injury by about 65%. For men without neurological injury, The American Cancer Society recommends laboratory prostate testing. The blood test, the prostate-specific antigen (PSA) is less predictive in men with SCI. If your PSA is consistently lower than 2.5 mg/ml, your healthcare provider may opt to only perform an annual prostate exam. If your PSA is higher than 2.5 mg/ml, your healthcare provider may perform additional testing. An annual prostate exam is still necessary.
Colorectal cancer has the same incidence in men with and without spinal cord injury.
Bladder cancer is only slightly higher in men with spinal cord injuries. The removal of latex in urinary equipment has greatly reduced the incidence of bladder cancer.
Gender Identity
Sexuality is unique to every individual. Gender includes a range, not just male or female. Some individuals have preferences that do not match any particular identification. For instance, some men enjoy the sensation of wearing women’s clothing. That does not mean they are of any specific sexual identity. Marketing has developed make-up for men which does not mean anything other than you want to enhance your look. Decide for yourself how you wish to identify as a human being. This is your choice. Sometimes people change or evolve their gender identity over time. Click here to find definitions of gender identities.
The Rehabilitation Healthcare Team
A physiatrist is a physician who specializes in physical medicine and rehabilitation. This individual will provide overall healthcare and direct therapy including sexual health information. They will direct you to the support services you request.
A general practitioner or internist medical doctor may be directing your general healthcare needs. This individual can also help you find the support needed for sexual health issues.
A urologist is a specialist in the urinary system which includes much of the same anatomy of the reproductive system. This individual can assist with questions or issues you may have.
A fertility specialist may be consulted if pregnancy is desired.
A genetic specialist may review your and your partner’s health history if a genetic issue is of concern.
A sexual health therapist or counselor can assist with issues with adjustment, performance, and techniques to create a satisfying sex life. This individual can help with becoming comfortable in relationships as well as presenting ideas for sexual satisfaction.
The physical therapist will assist with gross motor control, strengthening, positioning, and adaptive equipment for the goal of sexual activity.
An occupational therapist can assist with fine motor control, strengthening, positioning, and adaptive equipment with the goal of sexual activity.
The rehabilitation nurse will have a global view of the integration of all specialties to enhance sexual activity. This may include bowel, bladder, and skin issues as well as performance enhancement.
Research
A vast body of research is being conducted about human sexuality. This includes studies about individuals with paralysis. Sexual function is well documented including the natural desire for individuals with paralysis to want to continue their sexual life. Many studies about sexual dysfunction in men, in particular, erectile function have been conducted. Treatments have been developed to assist with erection. However, the issues concerning orgasm remain in achievement and intensity.
The evolution of functional electrical stimulation and nerve grafting has offered encouragement about the possibilities of improved sexual satisfaction. As the nervous system recovers through the development of nerve communication pathways, sexual function and sensation are demonstrated.
The continuation of fertility research has greatly enhanced the opportunity for individuals to become parents using their own genetic material. Advancements have made the process for many to be more intimate, in their own home without healthcare professionals and sterile clinical environments.
Facts and Figures:
Brain injury temporarily affects erectile function in 40-60% of men.
Spinal cord injury affects ejaculatory function in 95% of men. Some erectile function may return within two years of injury.
Multiple sclerosis affects erectile dysfunction in 50-75% of men, ejaculation and orgasm in 50% of men, and reduced libido in 39% of men.
There is an increased risk of sexual violence in individuals with disabilities.
Video: Men’s Sexual Health
Resources
If you are looking for more information about sexual health for men or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309.
Check out the Reeve Foundation’s repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
We encourage you to also reach out to support groups and organizations for individuals and families, including:
Model Systems Knowledge Translation Center: Sexuality and Sexual Functioning after SCI
Craig Hospital: Sexual Function for Men After Spinal Cord Injury
Mount Sinai Hospital: Sex, Love and Intimacy after Spinal Cord Injury
Centers for Disease Control and Prevention: Violence Prevention
Videos are available to assist in positioning:
Mount Sinai Hospital: Positioning with Partners
References
Baguley IJ, Barden HL, Nott MT. Altered Sexual Function After Central Neurological System Trauma is Reflective of Region of Injury; Brain vs Spinal Cord. Brain Inj. 2020 Dec 5;34(13-14):1732-1740. doi: 10.1080/02699052.2020.1832258. Epub 2020 Nov 15. PMID: 33190566.
Baird AD, Wilson SJ, Bladin PF, Saling MM, Reutens DC. Neurological Control of Human Sexual Behaviour: Insights from Lesion Studies. J Neurol Neurosurg Psychiatry. 2007 Oct;78(10):1042-9. doi: 10.1136/jnnp.2006.107193. Epub 2006 Dec 22. PMID: 17189299; PMCID: PMC2117556.
Barbonetti A, D’Andrea S, Martorella A, Felzani G, Francavilla S, Francavilla F. Risk of Prostate Cancer in Men with Spinal Cord Injury: A Systematic Review and Meta-Analysis. Asian J Androl. 2018 Nov-Dec;20(6):555-560. doi: 10.4103/aja.aja_31_18. PMID: 29956686; PMCID: PMC6219305.
Basson R. Human Sexual Response. Handb Clin Neurol. 2015;130:11-18. doi: 10.1016/B978-0-444-63247-0.00002-X. PMID: 26003236.
Brown DJ, Hill ST, Baker HW. Male Fertility and Sexual Function After Spinal Cord Injury. Prog Brain Res. 2006;152:427-39. doi: 10.1016/S0079-6123(05)52029-6. PMID: 16198718.
Cour F, Droupy S, Faix A, Methorst C, Giuliano F. Anatomie et Physiologie de la Sexualité [Anatomy and Physiology of Sexuality]. Prog Urol. 2013 Jul;23(9):547-61. French. doi: 10.1016/j.purol.2012.11.007. Epub 2012 Dec 31. PMID: 23830249.
Elliott SL. Problems of Sexual Function After Spinal Cord Injury. Prog Brain Res. 2006;152:387-99. doi: 10.1016/S0079-6123(05)52026-0. PMID: 16198715.
Ibrahim E, Brackett NL, Lynne CM. Penile Vibratory Stimulation for Semen Retrieval in Men with Spinal Cord Injury: Patient Perspectives. Res Rep Urol. 2022 Apr 21;14:149-157. doi: 10.2147/RRU.S278797. PMID: 35480782; PMCID: PMC9037179.
Karlsson AK. Autonomic Dysfunction in Spinal Cord Injury: Clinical Presentation of Dymptoms and Signs. Prog Brain Res. 2006;152:1-8. doi: 10.1016/S0079-6123(05)52034-X. PMID: 16198689.
Krassioukov A, Elliott S. Neural Control and Physiology of Sexual Function: Effect of Spinal Cord Injury. Top Spinal Cord Inj Rehabil. 2017 Winter;23(1):1-10. doi: 10.1310/sci2301-1. PMID: 29339872; PMCID: PMC5340504.
Merghati-Khoei E, Emami-Razavi SH, Bakhtiyari M, Lamyian M, Hajmirzaei S, Ton-Tab Haghighi S, Korte JE, Maasoumi R. Spinal Cord Injury and Women’s Sexual Life: Case-Control Study. Spinal Cord. 2017 Mar;55(3):269-273. doi: 10.1038/sc.2016.106. Epub 2016 Jul 12. PMID: 27401126; PMCID: PMC5791737.
Nout YS, Leedy GM, Beattie MS, Bresnahan JC. Alterations in Eliminative and Sexual Reflexes After Spinal Cord Injury: Defecatory Function and Development of Spasticity in Pelvic Floor Musculature. Prog Brain Res. 2006;152:359-72. doi: 10.1016/S0079-6123(05)52024-7. PMID: 16198713.
Papadakis JL, Zebracki K, Chlan KM, Vogel LC. Sexuality in Pediatric Spinal Cord Injury. Top Spinal Cord Inj Rehabil. 2017 Winter;23(1):42-48. doi: 10.1310/sci2301-42. PMID: 29339876; PMCID: PMC5340508.
Schmid DM, Hauri D, Schurch B. Nocturnal Penile Tumescence and Rigidity (NPTR) Findings in Spinal Cord Injured Men with Erectile Dysfunction. Int J Impot Res. 2004 Oct;16(5):433-40. doi: 10.1038/sj.ijir.3901188. PMID: 15014551.
Stratton MD, McKirgan LW, Wade TP, Vernava AM, Virgo KS, Johnson FE, Longo WE. Colorectal Cancer in Patients with Previous Spinal Cord Injury. Dis Colon Rectum. 1996 Sep;39(9):965-8. doi: 10.1007/BF02054682. PMID: 8797642.
Vogel LC, Betz RR, Mulcahey MJ. Spinal Cord Injuries in Children and Adolescents. Handb Clin Neurol. 2012;109:131-48. doi: 10.1016/B978-0-444-52137-8.00008-5. PMID: 23098710.



