Bowel Management
Bowel management is an issue for many individuals. Bowel issues range from constipation (where stool is too dry) to diarrhea (where stool has too much water) and every consistency in between. Many individuals have temporary bowel issues that pass within a short amount of time due to a temporary illness like the flu or an ‘upset stomach’.
Neurogenic bowel occurs with health concerns of chronic illness or trauma such as spinal cord injury, stroke, brain injury, Parkinson’s disease, myelomeningocele, amyotrophic lateral sclerosis, multiple sclerosis, sacral nerve injuries, diabetes mellitus or other neurological disease. Rarely, women can have neurogenic bowel issues after childbirth. Some individuals such as those with multiple sclerosis or diabetes have a bowel concern such as difficulty holding stool, but as their disease progresses, might evolve into neurogenic bowel. Those with a neurogenic bowel diagnosis can also concurrently have other bowel complications and diseases such as constipation, colitis, or irritable bowel syndrome among many others.
The Process of Digestion
Bowel management begins with the digestive process. The bowel is a part of the entire gastrointestinal (GI) system. Therefore, changes or adjustments to any part of the system will affect bowel function. When thinking about effective bowel management, the complete digestive system should be reviewed.
Digestion begins with smelling and seeing food which prepares your body for intake. The GI system begins with the mouth where food and fluid enter the body. The entry to digestion is the mouth. Saliva and chewing begin the process of digestion by breaking up food. Saliva secretions added to food and fluid further break down substances for digestion. Food and fluid are then swallowed and travel down the esophagus which is composed of a muscular and fibrous material that uses peristalsis (muscular contractions) to move food to the stomach. The esophagus typically passes food one way from the mouth to the stomach but can reverse when vomiting or with gastric reflux (heartburn). Food and fluid only pass through the esophagus. They are not held there.
In the stomach, food and fluid are temporarily stored as the next phase of digestion. There is a sphincter between the end of the esophagus and top of the stomach called the esophageal sphincter that closes to keep food from backing up into the esophagus. A sphincter at the bottom end of the stomach is the pyloric sphincter which helps hold food and fluid in the stomach temporarily.
During the time food and fluid is in the stomach, gastric fluids and acids continue the digestive process. The stomach is lined with ridges called rugae which cause muscular contractions to move the stomach contents around to ensure all the food is broken down into a semi fluid mass called chyme.
After the food is in the stomach for about two hours, the pyloric sphincter relaxes letting the chyme pass through to the duodenum or the top part of the small intestine, the next part of digestion. The duodenum continues to break down chyme for digestion using digestive enzymes from the liver, bile duct and pancreatic duct.
Helpful bacteria are normally in the bowel to break down chyme. These bacteria will not cause illness unless there is an opportunity to overproduce themselves. You can get an infection in your bowel, the same as you can from any other infectious bacteria. If you become dehydrated or have diarrhea, bacteria can flourish, overpowering the balance of helpful bacteria in the bowel.
The next part of the small intestine is the jejunum which continues the digestive process. The last part of the small intestine is the ileum. A complex set of very small blood vessels surrounds the front part of the duodenum and the entire jejunum and ileum. These blood vessels retrieve nutrients and fluid from the chyme as it passes through leaving mostly waste. The small intestine is made of a velvet like tissue which propels the chyme forward through the use of peristalsis or rhythmic muscle contractions of the intestinal wall. Most of digestion occurs in the small intestine.
Digestion is an ongoing process with the bowel only slowing at night while sleeping, but still processing chyme. The small intestine is curled up in the abdomen. In adults, the small intestine is about 22-25 feet long but has a small diameter to assist with propelling gooey chyme. A sphincter called the ileocecal valve, connects the small intestine to the large intestine. It is a one-way valve which prevents chyme from moving backward in the bowel.
The last part of the digestive system is the large intestine which consists of four parts the ascending colon, the transverse colon, the descending colon, and the sigmoid colon. The large intestine begins with wet waste in the ascending colon and removes water, bacteria, and salt as it travels through the other sections of the bowel turning the chyme into stool by removal of fluid. The large intestine is much wider in diameter than the small intestine because it is forming a soft, semi-solid stool for elimination. The length of the large intestine is about 2 1/2 feet. The same type of peristalsis (muscle contractions) action is used for propelling waste through it.
The end of the large intestine is the sigmoid colon, or rectal vault, which stores the stool until there is a socially acceptable time and place to empty. Two important sphincters help control the expulsion of stool. The internal anal sphincter is composed of smooth muscle tissue. It is about three inches from the opening of the rectum. The internal anal sphincter is not under your control (involuntary). This means it will open to let stool pass when there is a sufficient amount present in the rectal vault. The external anal sphincter is composed of striated muscle which is voluntarily controlled through use the pudendal nerves. If you feel the urge to have a bowel movement, you can control the external sphincter to hold stool until you find an acceptable location for expulsion.
Neurogenic Bowel
One of the main concerns for individuals with injury or disease affecting motor nerves (nerves for movement) is neurogenic bowel. This is a condition where the nerves of the body are not communicating effectively to and from the brain with the bowel. There can be a complete nerve transmission malfunction with no messages passing or just partial transmission of messages. Therefore, bowel management is essential for health.
Nerve Function in Digestion
Nerve function to the bowel is complex due to the length of this huge organ. The function of digestion is controlled overall by the Autonomic Nervous System (ANS). The ANS is the part of the nervous system that works automatically or without your voluntary control.
A plexus (branches of intersecting nerves) of nerves control movement in the esophagus, stomach, and intestines. Some of the nerves for digestion include the vagus nerve (cranial nerve 10) which also has some input to the stomach and upper bowel. The lower bowel is controlled by sacral nerves (S2, S3, S4) of the spine which includes the splanchnic nerve. Sensation of the external genitalia and skin around the rectum and perineum, motor supply to pelvic muscles, including the external anal sphincter is provided by the pudendal nerve.
Most of the work of the bowel is accomplished through peristalsis or rhythmic muscle contractions as directed by the vagus and splanchnic nerves, among others. When food enters the stomach, the gastrocolic reflex is stimulated which causes the bowel to increase movement intensity. The bowel is constantly working to remove fluid in the digestive process without thinking about it. With paralysis, the bowel tends to slow the peristalsis process. Even though the bowel slows its movement of chyme (digesting food) through it, the body is still removing fluid.
The farthest end of the bowel is controlled by specific nerves. Thoracic nerves T9-L2 reduce peristalsis while contracting rectal sphincters. Spinal nerves S2-4 will speed peristalsis while relaxing the rectal sphincters to release stool at the appropriate time and place to evacuate your bowel unless interrupted by neurogenic bowel. This is an efficient process when nerve messages are able to be transmitted.
Classification of Neurogenic Bowel
In the nervous system, communication occurs by motor nerves carrying messages from the brain to the body for movement. Sensory nerves carry messages of sensation from the body to the brain. This cycle is how messages are relayed. Moving your body is directed by the brain through motor nerves. Messages of sensation that something needs to happen to your body is sent to the brain by sensory nerves. Injury to the motor nerves creates a disruption resulting in neurogenic bowel. The source of injury, brain, spinal cord, or other neurological condition provides an indication of the type of neurogenic bowel function.
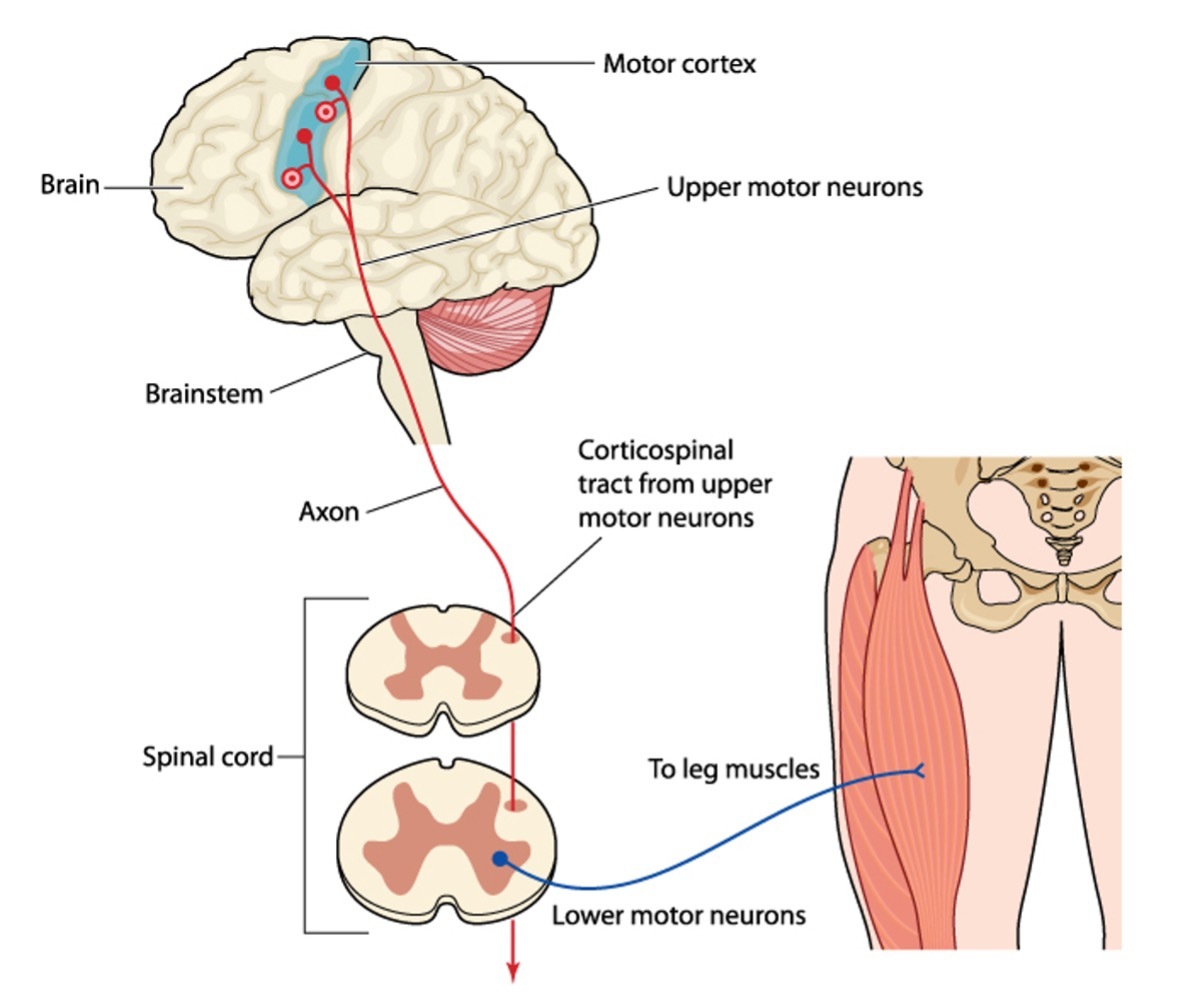
There are two types of motor neurons, upper motor neurons (UMNs) and lower motor neurons (LMNs). Although they share the same name, motor neurons, there are more differences than similarities.
| Differences | Upper Motor Neurons (UMNs) | Lower Motor Neurons (LMNs) |
|---|---|---|
| Neurotransmitter | Use glutamate to send messages to LMNs | Use acetylcholine to send messages to the muscles |
| Target of transmission | Within the Central Nervous System | In the body |
| Cell bodies | UMNs are within the brain. They are the source of movement. | LMNs are in either the brain stem or spinal cord. They are the connectors between UMNs and the target muscle for movement. |
| Muscle atrophy (wasting) | Minimal–because they connect to LMNs (muscle targets are indirect) | Severe-because they directly target muscles |
| Muscle Affect | Hypertonic (spasticity) | Hypotonic (Flaccid) |
| Subtypes of Motor Neurons | Only one type: Upper Motor Neuron because they are only in the Central Nervous System. | Three types depending on the target muscle type:
-Branchial motor neurons which innervate the face and neck through five of the cranial nerves (CN): (CN V) trigeminal (CN VII) facial (CN IX) glossopharyngeal (CN X) vagus (CN XI) accessory nerve -Visceral motor neurons which control the smooth muscles of the internal organs and glands -Somatic motor neurons that innervate skeletal muscles for movement. There are three types, one for each of your muscle types: Alpha–cardiac muscle Beta–smooth muscle found in body organs Gamma–skeletal muscle |
Upper Motor Neurons and Lower Motor Neurons
Types of Neurogenic Bowel
Neurogenic bowel is classified in three ways.
Reflexic/Upper motor neuron (UMN) neurogenic bowel is diagnosed in individuals with an injury or disease affecting upper motor neurons. Reflexic (UMN) bowel results from injury to motor nerves above the conus medullaris (L1 or L2). In spinal cord injury, reflexic (UMN) neurogenic bowel is typically at the cervical or thoracic levels.
The bowel and internal rectal sphincter are hyperreflexive or spastic (tone). Because of spasticity (tone), the anocutaneous reflex (contraction of the anal sphincter by stimulating the surrounding skin) and bulbocavernosus reflex (assessment of S2-4 function) are present or increased. This causes the bowel to retain stool, with only small amounts spontaneously released due to spasms (tone). Not all stool will be expelled leading to involuntary small bowel movements at erratic times. A bowel program using stimulation is initiated to empty the bowel completely at a predictable time.
Areflexic/Lower motor neuron (LMN) neurogenic bowel results from injury or disease affecting lower motor neurons (LMNs). In spinal cord injury, the motor neuron injury is typically in the lumbar or sacral area or below the conus medullaris (L1 or L2).
This bowel and internal rectal sphincter are flaccid or ‘areflexic’ meaning tone is low to absent. The anocutaneous reflex (contraction of the anal sphincter by stimulating the surrounding skin) and bulbocavernosus reflex (assessment of S2-4 function) are low functioning or not present. Stool will collect in the rectum without spontaneous evacuation (no reflex release). The flaccid bowel does not respond well to stimulation. If the lower bowel becomes full of stool, the bowel will stretch to accommodate the overload. However, at times, a small amount of stool might be released as incontinence because of absence of tone in the rectal sphincters or there is no more room in the bowel, but a large amount of stool remains. The stool remains in the rectum with water constantly being removed so it becomes very dry and hard. In an areflexic (LMN) bowel, stool is manually removed during the bowel program.
Mixed motor neuron bowel is a mixture of injury to upper motor neurons and lower motor neurons. Individualized plans for bowel evacuation using strategies for reflexic (UMN) and areflexic (LMN) bowel evacuations are established depending on the function of the mixed neurogenic bowel.
Diagnosis of reflexic (UMN), areflexic (LMN), or mixed motor neuron bowel is treated with a bowel program to safely and effectively remove stool, to avoid social embarrassment and skin breakdown and to keep stool from backing up into the bowel leading to impaction or nausea and vomiting of stool.
Table 1 – Features of Upper Motor Neuron (UMN) versus Lower Motor Neuron (LMN) Bowel Dysfunction
Reprinted with permission. Credit: PM&R KnowledgeNOW https://now.aapmr.org/neurogenic-bowel/
Diagnosis of Neurogenic Bowel
Causes of neurogenic bowel can include any disease or trauma to the brain, spinal cord or peripheral nerves (nerves outside of the Central Nervous System (CNS)). Disease sources can begin as issues with bowel function and progress to neurogenic bowel whereas neurogenic bowel onset from trauma is typically sudden. Indications of the presence and type of neurogenic bowel is often first identified by medical diagnosis or trauma.
Neurogenic bowel diagnosis includes a history and physical examination. Your healthcare professional, a neurologist or a specialist in physical medicine and rehabilitation (physiatrist) will perform the examination. This includes a history of symptoms, gastrointestinal issues both in the past and now, bowel habits (frequency, consistency, flatus (gas), incontinence, time spent in toileting, fecal impaction, laxatives or antidiarrheal use, diet, fluid intake, activity and limitations on quality of life. Details of current toileting assistance, medications and aids should be described.
Physical examination consists of an assessment of the entire abdomen area. A digital rectal examination will be performed which provides an assessment of rectal filling, resting anal tone, reflexes, and ability to produce a voluntary contraction. Evaluation of the anocutaneous reflex (contraction of the anal sphincter by stimulating the surrounding skin) and bulbocavernosus reflex (assessment of S2-4 function) discriminates between the types of neurogenic bowel.
An X-ray of the abdomen will indicate the amount of stool present, blockages, or other structural issues in the bowel. Retaining stool is one sign of neurogenic bowel.
Transit time is an assessment of the amount of time for food to travel through your body from eating to expulsion and can be assessed with radiopaque markers (x-ray landmarks), scintigraphy (use of isotopes) or an electronically transmitting ‘pill’. Average transit time without neurogenic bowel is 20-56 hours. Slower transit times can indicate neurogenic bowel.
Muscles of the pelvic floor including sphincter, anus and rectum can be assessed using anorectal manometry. A colonoscopy prep is performed prior to the procedure. A flexible catheter with sensors measures pressures while you contract and relax your rectum. Lower pressures can indicate neurogenic bowel.
Bowel issues have been noted to affect an individual’s quality of life and mental well-being. A reliable and valid assessment instrument, the Spinal Cord Injury-Quality of Life (SCI-QOL) measurement system, contains a section to assess the impact of bowel issues on quality of life. This questionnaire contains statements about the impact of bowel issues rated on a five-point scale from ‘not at all’ to ‘very much’. SCI-QOL questions and instruments are copyrighted by David Tulsky and the Kessler Foundation with all rights reserved.
The medical evaluation may include other assessments and tests such as a neurological examination, an EMG (electromyogram) or NCS (nerve conduction study), CT Scan or MRI. After an injury to the nervous system from trauma or a medical condition, there are often disruptions to the motor neurons and sensory neurons. Establishing a diagnosis of the source of the issue is important to understanding the type of neurogenic bowel that is present.
The International Standards of Neurological Classification of Spinal Cord Injury (ISNCSCI, also known as ASIA or the ASIA Impairment Scale (AIS)) has a section for assessment of bowel nerve function. The ISNCSCI examination flow sheet can be seen here. The last section of the ISNCSCI exam includes an assessment of urinary and rectal function. The ISNCSCI examination should be performed yearly to assess for changes in condition and complications.
How to Talk about Stool
Being able to discuss stool frankly and openly with your healthcare professionals and caregivers is essential to obtaining the treatments you need. Some individuals are hesitant to discuss bowel movements. The Bristol Scale is a standard language to describe stool using consistent terminology.
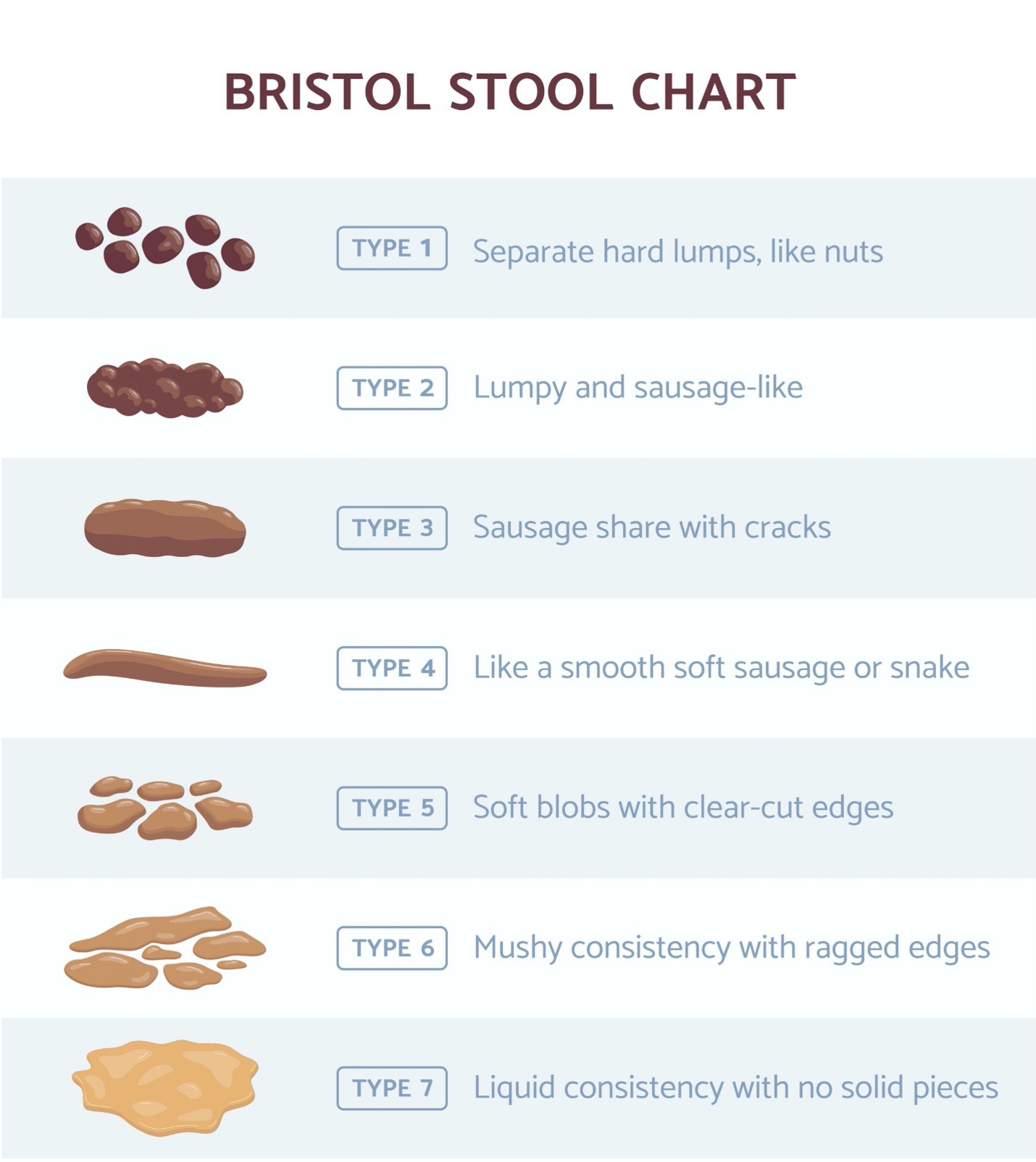 A stool diary is helpful to track consistency and timing of your bowel movements. This is a tool to share with your healthcare provider for treatment decisions. If you have multiple healthcare providers and caregivers, they can also review your patterns. There are many options available without charge. They can be downloaded from your app store.
A stool diary is helpful to track consistency and timing of your bowel movements. This is a tool to share with your healthcare provider for treatment decisions. If you have multiple healthcare providers and caregivers, they can also review your patterns. There are many options available without charge. They can be downloaded from your app store.
https://bristolstoolchart.net/
https://careclinic.io/stool-tracker/
https://apps.apple.com/us/app/stool-log-lite/id782394941
Rehabilitation for Neurogenic Bowel: The Bowel Program
Establishing a bowel program is the treatment for neurogenic bowel at any age from birth through adulthood. Bowel programs are designed to work in the intestine and rectum to parallel natural bowel movement and evacuation. The goal of a bowel program is to expel or remove stool from the body in a safe and efficient manner with no breakthrough incontinence.
Overall Bowel Program Guidelines:
- Consistency in timing is critical to success. An established time to perform a bowel program will ‘train’ the bowel to empty on a regular routine. Most people without a spinal cord injury have natural elimination habits that develop over time. The same will also happen for those living with a spinal cord injury but cues are needed to be provided as to when elimination should occur. The bowel program accomplishes this timing.
- Take advantage of the gastrocolic reflex (stimulation of bowel function from eating). It is strongest at the first meal of the day but can be stimulated with any meal or snack.
- Warm fluid can stimulate the bowel to function.
- Gravity assists with bowel evacuation. Sitting upright using the toilet or a commode aids in elimination. Gravity will help bring the stool to the rectal vault as well as out with digital stimulation or manual removal. If the bowel program must be performed in bed due to a medical reason, laying on the left side will anatomically help facilitate the process.
- Internal and external factors affect the bowel. Become aware of things that affect bowel function such as illness, specific foods and fluids, activity, and mental health.
- When cleaning after a bowel movement, use toilet tissue, mild soap and water or wet wipes to remove any residue that you may or may not see around the rectal area. Dry carefully and thoroughly to maintain your skin integrity.
Reflexic/Upper Motor Neuron Neurogenic Bowel Program
Be aware that autonomic dysreflexia (AD) can occur in individuals with reflexic (UMN) neurogenic bowel.
For individuals with reflexic/(UMN) injury or injury in the cervical and thoracic spinal cord, a typical bowel program includes a stimulant followed by digital stimulation at the same time every other day.
Using a lubricated, gloved finger, check the rectal vault to be sure stool is not blocking the bowel. If stool is present, very gently remove it so the stimulant can reach the bowel. Insert the stimulant gently against the bowel wall about 20 minutes after eating to take advantage of the gastrocolic reflex.
Stimulants used are a suppository or mini enema. Most individuals use a suppository, bisacodyl (Dulcolax) or Magic Bullet for adults, glycerin for children or elderly. If a suppository appears to be too strong as indicated by harshness, cramping or excessive mucous discharge, it can be cut long ways in half. Some individuals prefer use of a mini enema (Enemeez or Therevac) as they feel it provides quicker and more efficient results. Full enemas are not used because they do not mimic or stimulate natural bowel function. Suppositories and mini enemas are effective when placed against the bowel wall. If the suppository or mini enema is placed in the center of stool, it will not melt or stimulate peristalsis or movement of the bowel.
Move to a commode or toilet after insertion of the stimulant in about 15-20 minutes, you will learn the amount of time needed prior to your suppository beginning to work. Then begin digital stimulation. Digital stimulation should be done gently for 10 to 20 seconds, 5-10 minutes apart, up to four times, until stool is expelled.
The purpose of digital stimulation is to accelerate bowel function and to relax the internal sphincter which is held closed due to spasticity (tone). These actions allow the stool to pass. The external sphincter can be seen while the internal sphincter might be felt when the finger is inserted. Be sure to use enough lubricant to create a smooth pass along the full length of your finger. This should be a calm movement as aggressive action will increase spasticity. If finger and hand function are difficult, adapted rectal stimulators and inserters can be purchased.

Areflexic/Lower Motor Neuron Program
Individuals with areflexic (LMN) injury usually in the lumbar or sacral spinal cord have a flaccid bowel and sphincters (absent rectal reflexes) therefore typically do not respond to stimulants or digital stimulation. The bowel program consists of manual removal of stool using a well lubricated, gloved finger. Insert a lubricated, gloved finger into the rectum. Use a ‘hook’ like motion to release stool.
To prevent injury to the delicate bowel tissue, lubricate the entire length of the finger. Try to break up stool internally for easier passage. Depending on your bowel function, gently remove stool daily, or more frequently. Many individuals check their bowel several times during the day to ensure continence.
Mixed Motor Neuron Bowel Program
The technique for a bowel program with mixed motor neuron issues will be use of either of the reflexic or areflexic bowel programs or a combination of techniques used in motor neuron bowel programs. This will be individualized to your specific needs.
Changes in Neurogenic Bowel Program Techniques
In the past, abdominal bowel massage and Valsalva (straining) were techniques that were promoted for stool evacuation. However, complications of hemorrhoids, abdominal pain, anal fissures and rectal prolapse were noted with these techniques. Valsalva is also a factor in urine reflux (backup) into the kidneys. Therefore, these techniques are no longer recommended. If you are using these options, check with your healthcare professional to assess their continued use in your bowel program.
Changing your Bowel Program Schedule
Consistency in timing is the rule for training the bowel to work effectively. However, sometimes life changes and a new schedule is needed. Changing your bowel program should not occur very often as consistent timing is needed for your bowel program to work. However, on that rare occasion, it is possible to change your bowel schedule.
Start your bowel program at your newly selected time. Stop, your usual program. Perform the bowel program at the new time daily until stool is evacuated on the new schedule for 2-3 days or a week with no incontinence in between. You may not have results daily and might have bowel incontinence around your original bowel program time. Even with incontinence, perform the bowel program at the new time. When you reach a point of no incontinence between daily bowel programs, usually between 2-3 days or a week, you can move to every other day at the new time. It can take weeks or sometimes a month to regulate your bowel to the new schedule, but success will happen. Accidents in between can be frustrating so be prepared for that consequence.
Neurogenic Bowel Issues
Most people think of the bowel program as just being the process of elimination of waste from the body. But it is really a 24/7 process. These are other considerations of the total bowel program process.
Autonomic Dysreflexia
Individuals with a spinal cord injury above T6 (or even as low as T10) can have bouts of autonomic dysreflexia with their bowel program. The second cause of AD, behind bladder issues, is bowel concerns such as an overfilled bowel, diarrhea, gas, impaction or even due to the stimulation of the bowel program itself.
The most common signs of AD are a pounding headache and elevated blood pressure which is higher than your individual normal. There are other signs as well. Sometimes silent AD can be occurring which is an elevated blood pressure with no other symptoms. Be well aware of all of the signs of AD by checking the AD wallet card.
AD is a serious medical emergency that requires attention. If you have multiple episodes of AD with your bowel program, medication can be prescribed to control AD as well as a topical rectal anesthetic to control the bowel program as an AD trigger.
Aging
Bowel programs may function well for years without any issues when, for no apparent reason,that changes. Part of the issue can be the effects of long-term neurological issues and aging. As individuals age, the bowel can slow. Combined with the bowel challenges of neurological issues this can be a compounding complication.
Starting from the beginning might help in creating an improvement. Review your diet, fluid intake, medications, and activity level. Talk with your healthcare professional to review your techniques and medications. Sometimes people get caught in a cycle of adding things to make the bowels move and adding other things to stop it. Let the bowel do its natural processing with minimal intervention if possible.
Bowel nerve function
Individuals with neurological issues have difficulty with their bowels because of slowing of the bowel function by the nerves of the Autonomic Nervous System (ANS). This nerve system slowing combined with decreased body movement affects bowel function.
Many people think that because the bowels are slow, the problem is constipation. This is not the source of the problem. Treatment for constipation will not assist a neurogenic bowel to work more efficiently. Individuals with or without neurogenic bowel can become constipated. Neurogenic bowel does put you at higher risk for constipation. A bowel program will result in controlled bowel movements with a neurogenic bowel.
Bowel with Sensation
Individuals with neurologic disease, incomplete spinal cord injuries or with partial preservation of some nerves may have some sensation in the rectal area causing discomfort with the bowel program. Messages may be transmitted that something is going on in the bowel or messages can be mis-transmitted as pain. A first line treatment is to use a rectal topical anesthetic at the time of the bowel program. This analgesia can be inserted prior to the initiation of the bowel program or it can be used as lubricant, depending on your specific needs. If there is no success with this treatment, neuropathic pain medication, spasticity (tone) medication or other treatment may be necessary.
Bulk Fiber
Fiber building powders, cookies and wafers have been initiated for many individuals with neurogenic bowel to increase bulk in chyme and stool with the goal of propelling these through the bowel. These products require eight ounces of fluid to be consumed to be effective. Without adequate fluid, the bulk fiber tends to harden the chyme and stool which can lead to slower bowel function, more difficulty in passing the waste and even to impaction. Therefore, fiber building products are not being prescribed for those with reflexic neurogenic bowel. Individuals with areflexic neurogenic bowel can continue with bulk fiber use as long as including the recommended fluid.
Many individuals with neurogenic bowel may also be monitoring their fluids for bladder management, heart conditions, extreme edema, or other health issues. Because it is a contradiction to control fluids for one health issue and increase fluids at the same time, bulk fiber is no longer an automatic recommendation for those with fluid restrictions. It has been found that most individuals will process chyme and stool without the conflict of the bulk fiber.
Check with your health professional to see if you should continue with bulk fiber. Some healthcare professionals might recommend it but with divided doses so water intake can be achieved. If you are having constipation issues, discuss a plan with your healthcare provider for switching to alternative treatments such as a change in diet or stool softener, among others.
Colonoscopy
When a person reaches their 45th birthday, a gift from your healthcare provider will be the recommendation of a colonoscopy. Colon and rectal cancer are the fourth most common cancer.
The symptoms of bowel and rectal cancer can be hard to detect. If you have had any kind of cancer, bowel inflammation such as colitis or Crohn’s disease, polyps in the bowel or eat a high fat diet, you are at risk. There appears to be a genetic factor for colon and rectal cancer. Risk is increased if someone in your family has bowel or rectal cancer. One of the major risk factors for colon and rectal cancers and other types of cancer is cigarette smoking. Manage risk factors by eating a diet high in fiber and stopping smoking. Giving up smoking, chew, vaping, e-cigs and reducing exposure to second hand smoke will help reduce cancer risks. Inherited factors can be managed but not eliminated.
Symptoms of colon and rectal cancer might be feeling tired, blood in the stool, excessive bloating, gas, feeling that your bowel does not empty, nausea and vomiting. Stools that are very thin in width can indicate a blockage which may or may not be cancer. These symptoms can all be signs of other problems as well. Therefore, it is good to have these issues checked out by colonoscopy if they are persistent.
Most individuals will be sedated during the colonoscopy. You will not know it is even happening. Sometimes, you might be told that you will not feel the procedure because of your spinal cord injury, however, your body will still respond to the procedure. Light sedation should be provided. Discuss sedation possibilities with your healthcare professional who provides care for your neurological issue as well as the person performing the procedure to see what will be right for you.
Autonomic dysreflexia (AD) is a concern during the colonoscopy prep and procedure. It typically occurs in individuals with SCI above T6, however, it has been noted in some people with injury levels as low as T10. You may have never had an episode of AD until the prep or colonoscopy procedure. Both the prep and the procedure can trigger an episode. Careful monitoring is required during the prep and the procedure. More information is available at: https://www.ChristopherReeve.org/cards
In preparing for the colonoscopy, your bowel needs to be clean so that the person performing the procedure can clearly visualize the bowel wall. The preparation for a colonoscopy varies by examiner. There are many products that are used to cleanse the bowel. Follow the instructions specifically provided.
Check with your healthcare professional about hospitalization prior to your colonoscopy. Some payors will cover this option especially if you are at risk for AD, must be on a longer clear liquid prep, and need assistance with the bowel cleanse.
Resume your bowel program routine as instructed by your healthcare professional. Most people will resume their bowel program within the next day or two. Keep your bowel program working.
Constipation
Anyone can become constipated with or without neurogenic bowel. Constipation is stool that is too dry. The cause can be from too slow of a transit of chyme and stool through the bowel or not enough hydration in the body or both. Slow transit time through the bowel or lack of fluid will dry stool as the entire time chyme and stool are in the bowel, water is being extracted. Constipation can also be caused by a stricture or narrowing of the bowel, colon cancer or other structural issue.
Sometimes, people have a temporary constipation. Temporary causes of constipation include being out of routine and not taking in enough fluid one day, over drinking alcohol which will dehydrate the body or exercise or work with an overproduction of sweat. People become dehydrated for a variety of reasons, even illness such as fever. The result is seen in your stool which becomes very dry.
Treatments for constipation include fluid (if not on fluid restriction), diet of unprocessed foods, body movement or activity, and stool softening medications. If you have temporary constipation, you might not need to change your typical routines. Individuals with neurogenic bowel issues may need to increase some of the above listed treatments. To increase treatments, add just one item at a time and wait awhile for results. Changing all at one time or adding too quickly can lead to diarrhea episodes.
Diabetes
Diabetes is a disease that can affect nerves of the bowel. Eating food containing large amounts of carbohydrates and sugars will result in loose stools or diarrhea when the sugar hits the bowel. Since diabetes affects nerve function, over the long term, diabetes can affect the nerves to the bowel and within the bowel leading to slower bowel movement and eventually bowel dysfunction. If you have diabetes, follow your diet, take prescribed medication, and add activity or movement into your lifestyle. If you notice your bowel program becoming slower or less effective, it is time to discuss alternatives with your healthcare professional.
Diarrhea
Diarrhea seems to come for no apparent reason and certainly will appear at the least opportune moment. It can be caused from a bacteria or virus in the bowel, diseases such as diabetes, and changes in physical and mental wellness. Diarrhea is a result of stomach flu, any gastric illness or just from how our bodies react with certain foods. Diarrhea can also come from stress. The bowel is programmed to eliminate when a person is frightened which is the same process as stress.
Diarrhea will typically resolve when the illness is over or when you are no longer under stress. Remember, happy, exciting events can be stressful, also. If severe diarrhea appears, you can skip your bowel program for that day if you feel your bowel is completely empty. Then return to your routine. If the diarrhea is prolonged, you will need to see your healthcare professional to get to the source of the issue and to avoid dehydration.
Antidiarrheal medication can be taken but use with caution. Antidiarrheals slow the bowel which makes return to your normal function slower. Rectal bags can be worn to keep the caustic diarrhea stool off your skin. Washing with soap and water will clean your skin but is drying. Use skin prep or lotions containing zinc oxide to protect skin and help to keep it intact.
Diet
Eating a healthy diet is key to your general health as well as to bowel function. A person with neurogenic bowel often does not feel hungry because the slow bowel creates the sensation of fullness. Changing your eating habits will have an impact in a bowel program.
The daily fiber requirement for individuals under 50 years is 25 grams for women and 38 grams for men. After age 50, people tend to eat less on average, so the fiber requirement is lower, 21 grams for women and 30 grams for men. One of the top changes should be to reduce your intake of processed foods. Instead eat fresh items, especially produce. This adds a tremendous amount of fiber to your diet.
There are certain foods that help move stool through the bowel. Beans have a pronounced effect on the bowel because of their fiber content. You can easily slip them into other dishes such as adding them to salads, casseroles, soups, stews or just as a side dish. Do not forget beans are popular as dips with fresh vegetables. Other fiber rich foods are lentils, cooked potatoes, squash, seeds and nuts, bran, broccoli, cauliflower, cabbage, peas, and celery. Cereals are designed to add fiber. Just be sure to check that the sugar content is not high.
Individuals with neurogenic bowel can develop a secondary complication of diabetes due to a variety of factors including lack of movement in their bodies. Limit carbohydrate and sugar intake as once the diabetic bowel senses sugar in any form, it tends to spontaneously speed its work which can lead to incontinence. You do not have to eliminate sugar and carbohydrates, just eat them in moderation or according to a diabetic food plan.
Digital Stimulation
A technique for individuals with a reflexic (UMN) neurogenic bowel is digital stimulation. The goal of digital stimulation is to relax the inner sphincter and to trigger bowel function. The inner sphincter is about three inches from the rectal opening. You may or may not feel the inner sphincter relax with digital stimulation, but a gentle process close to the inner rectal sphincter will relax spasms (tone).
Aggressive digital stimulation can slow the bowel elimination process by increasing spasms (tone in the inner rectal sphincter). Gentle digital stimulation using lubricant can avoid triggering spasms, tearing delicate bowel tissue, hemorrhoids, and other bowel issues. Gentle removal of stool also avoids these issues.
Some individuals cannot perform digital stimulation due to heart conditions or severe autonomic dysreflexia (AD). If your cardiologist or healthcare professional recommends no digital stimulation, you may still be able to perform a bowel program, but you will need specific instruction from your healthcare professional which might include use of a topical rectal anesthetic.
Diverticulitis
Diverticulitis is the development of small pouches along the wall of the bowel which can become infected and inflamed. How the small pouches develop is unknown but there is some evidence that they develop from weakened spots along the bowel. Allowing stool to collect in the bowel without a bowel program for elimination can supply pressure to the bowel wall. Diverticulitis can lead to pain, discomfort, bleeding and even eruption which allows stool to enter the abdomen.
Symptoms of diverticulitis are pain if sensation is intact, fever and chills if the bowel becomes infected, an increase in bloating and gas, diarrhea or constipation, nausea and vomiting or not feeling like eating. Diagnosis of diverticulitis is made though x-ray or colonoscopy. If you do develop diverticulitis, antibiotics can treat small infections. If the infection becomes an abscess or a large pocket of infection, it may have to be drained. Fistulas can develop if the bowel attaches itself to another part of the bowel or another body part.
Prevention of diverticulitis is achieved by eating a high fiber diet to move waste through the bowel more easily. Adding water to your routine will help moisten your stool. Maintaining your bowel program routine is imperative.
Emotions
Anxiety, stress, nervousness, happiness, being upset, or just a change in your daily routine can affect the bowel program. Your mental wellbeing affects your bowels. Everyone has good days and disastrous days which will affect your bowel function. Ongoing stress and other mental wellness should be addressed with therapy to gain skills in dealing with challenges.
Enema
Full enemas should not be routinely used for neurogenic bowel management because they do not mimic the natural action of the bowel. Instead, they wash out the bowel reducing healthful bacteria. If the bowel does not perform its rhythmic motion, the function eventually becomes weaker leading to even more difficulty in completing the bowel program. Mini-enemas (Enemeez or Therevac) work only in the lower bowel or rectal vault. These are appropriate as alternative stimulants for bowel programs.
Fluid
Additional fluid helps to keep chyme and stool moist for the entire length of the bowel. Check with your healthcare professional to see if you can increase your fluid intake. A bladder program, heart conditions, and some instances of excessive edema among other diagnoses can lead to fluid restrictions.
Increasing fluids should start slowly. Taking in large amounts of water too quickly can overload your entire body system and even lead to incontinence. Small sips throughout the day is the best way to increase your intake of water. You do not need to increase by cups of fluid quickly, increase slowly, just a sip or two at a time. A sip or two every hour when you are awake can add fluid to help your bowel function.
Water is the best option for keeping a moist stool. Consider the effects of other liquids. Alcohol causes dehydration that affects stool as well as the rest of your body. Caffeine can also dehydrate. Sugary and artificially sweetened drinks will cause the stool to move more quickly through the bowel. You can still enjoy these drinks, just use them in moderation.
It is important to keep up with your fluid intake to keep your bowels moving efficiently and effectively. If you have the ability to sweat, you may need to take in a bit more fluid such as on a hot day. Do not forget humidity can dry your body without sweating even if the temperature is not high. In the winter, you can dehydrate from being in a room with dry heat.
Functional Electrical Stimulation (FES) and Epidural Stimulation
Electrical stimulation can be applied to the body through electrodes placed on the skin. Electrodes placed on the abdomen may have an impact on bowel function, but this is still being explored by research. FES to other parts of the body, such as the legs, helps stimulate the bowel through body activity.
Epidural electrical stimulation occurs using implants in the body. This is an emerging field of study. Preliminary results indicate improvement in bowel function with this technique.
Sacral anterior root stimulation (SARS) and sacral nerve stimulation (SNS) are implants for stimulation of the sacral nerves with improvements in bowel function and continence. These implants are currently directed for individuals with areflexic (LMN) neurogenic bowel.
Gas
Bloating and gas can be an issue for individuals with neurogenic bowel. Slowing of the bowel can lead to a buildup of gas which appears as bloating. Movement can help resolve some of the issue because it pushes gas along in the bowel. Eating foods that produce little gas can help. Adding movement through range of motion exercises, pressure reduction techniques and activity assist with gas movement in the bowel.
Gas reducing tablet medication (simethicone) is available. Take gas reduction medication when needed, not as a routine, if possible. Gas in the bowel is one of the ways waste is propelled through the bowel. It is a necessary action. Eliminating gas can reduce bowel propulsion.
Gravity
Gravity is often overlooked as one of the biggest aids in bowel movements. You might have been taught to do the bowel program in bed. However, sitting upright will help stool pass from your body by taking advantage of gravity.
To accommodate sitting, request a commode chair or shower chair which can be dually used for your bowel program. Have your therapist, nurse or healthcare professional assist you with ordering your commode to ensure you have all the adaptions needed specifically for you such as appropriatebrakes, removeable and elevating foot rests, removeable arm rests, head rest, reclining feature, appropriate padding for skin care and safety belts. Be sure the size of the commode can be accommodated in your home and doorways. Check with your insurance case manager to learn about the payment system.
If you have a medical reason that you cannot sit up for the bowel program, position yourself on your left side. The bowel program will be more effective in bed if you are on your left side due to the anatomical placement of the bowel within the body.
Hemorrhoids
Hemorrhoids are dilated vessels of the rectum. Sometimes, they are internal where they might not be seen but felt, or they are external where they can easily be seen. Hemorrhoids are not particular to those with neurogenic bowel. They are most often caused in the general public by hard stools and straining to pass stool. Sitting for extended periods of time on the toilet or commode without pressure support to the rectal area is another cause. For those with neurogenic bowel, overzealous and poor lubrication of digital stimulation can increase development of hemorrhoids.
Symptoms of hemorrhoids are rectal bleeding, pain, burning, and itching or have an onset of autonomic dysreflexia (AD) or increased spasticity (tone) as your body tries to tell you something is wrong below the level of injury. The presence of blood or visually seeing external hemorrhoids may be your symptoms if you have sensation issues. Blood typically will appear on the outside of the stool, not within it because the hemorrhoids are at the area of expulsion.
Many people think a bowel program will automatically cause hemorrhoids, but this is not necessarily the case. Bowel programs can be successfully completed without the development of hemorrhoids. With sensation issues, it might not be noted that there is not enough lubricant on the gloved finger to perform these delicate procedures. Sometimes the lubricant slips off the finger before it can be inserted. Making sure the lubricant is present for the length of the finger is imperative.
The other issue is technique. Gentle digital stimulation and gentle manual removal reduce hemorrhoid risk. The idea of completing the digital stimulation is to dilate or relax the internal sphincter to open to let the stool pass. Often people are gouging at the rectum. This is not necessary. A gentle, circular motion, feeling for the internal sphincter and noting it relax, will accomplish this job. Removal of hard stool is difficult. It strains blood vessels in your rectal area which can result in hemorrhoids and can even lead to tearing. Water intake and stool softeners can assist with easier stool removal.
Sitting for long periods of time or straining when using the toilet can increase your risk of hemorrhoids. Toilet and commode seats do not provide support to the rectal area but rather allow your upper body weight to be resting in the unsupported rectal area. Position yourself on the toilet or commode just for digital stimulation and evacuation.
Detection of a hemorrhoid should be noted and treated early. If hemorrhoids become present, you can reinsert them with your lubricated, gloved finger to keep them moist by using your body’s own internal fluids. Use of hemorrhoid ointment will help reduce swelling and inflammation. Rectal cooling pads will help control pain and itching of the hemorrhoid. Stool softener medication taken by mouth will coat stool for easier passage.
Bleeding from the rectum can be a serious healthcare concern. You may need a colonoscopy to determine the source of the bleeding which can be other, more serious, bowel conditions. Should you have significant hemorrhoids or complications, you can have them removed by a choice of several techniques. Conservative treatments are best but if removal is required, non-excision techniques should be performed.
Impaction
An impaction occurs when stool gets ‘stuck’ in the bowel. Impactions can be due to a variety of health factors, not necessarily poor bowel care. Absence of bowel program results, nausea, and vomiting, or an enlarged or hard abdomen are signs of a bowel impaction. Watery stools may be oozing around an impaction.
If stool is low in the bowel a digital check will identify it. If the impaction is higher in the bowel or if the problem persists, an X-ray is done to assess for impaction. Manual removal may have to be performed to resolve this situation if the impaction is in the rectal vault. Impactions higher in the bowel require sequential enemas for removal. Disimpaction may be needed to be performed by healthcare professionals to reduce complications of lowered blood pressure, autonomic dysreflexia (AD) and damage to the bowel.
Stool softening medication, fluid and activity will help keep the stool moveable. Adherence to a bowel program so stool does not linger or dry in the bowel is necessary.
Injured Bowel
Too infrequent bowel programs, gas, impaction, aggressive digital stimulation or aggressive manual removal of stool can lead to injury to the delicate bowel tissue. Hemorrhoids, fissures, fistulas, diverticula and overstretching of the bowel can occur. Treatments for injury to the bowel depend on the source and severity. Be gentle when doing a bowel program as well as use generous amounts of water-soluble lubricant.
Insertion of suppository or mini enema
For bowel stimulants to work, gentle placement next to the wall of the bowel is required. Stimulants will not function if they are inserted in the middle of stool. It takes body heat for suppositories to melt. Stool is not warm enough. The suppository and mini enema work by stimulating the bowel so they must have contact with the wall of the bowel to function. If stool is present in the rectal vault, it must be removed prior to insertion of a stimulant.
Latex
A substance that used to be found in medical products especially in rubber supplies such as gloves and catheters is latex. It was the source of extreme allergies and even cancer especially when it repeatedly touched mucous membranes such as the bowel or urethra. It has been removed from medical products. Be sure to check supplies for ‘non-latex’ and dispose of them to avoid latex allergy and other complications.
Laxatives
Avoid laxatives as they produce irregular results and timing of bowel movements that cannot be controlled leading to bowel incontinence. Over time, the bowel will rely on laxatives to stimulate movement, reducing natural bowel function.
Movement
Movement helps everyone’s bowels to work more efficiently and functionally. People who live sedentary lifestyles even without neurological issues have more difficulty with bowel movement than those who move their bodies.
There are some simple activities that will insert movement into your life. Roll from side to side when in bed, perform pressure releases, do range of motion exercises especially to the legs and hips, exercise especially the lower body or have someone do these activities to your body. Since the bowels are inside the body, we do not see them moving but muscle action helps propel stool through the bowel. Therefore, supply what is needed to enhance the process.
Mucous and other discharge after Bowel Program
Mucous production after a bowel program is often a concern for individuals. In this situation, the bowel program is complete but mucous is evacuated at the end of the bowel program or sometimes hours later. This is a particular issue for those who use bowel stimulants. At times, a stimulant can still be exciting the bowel even though stool has been evacuated. This results in the expulsion of mucous.
There are several ways to manage mucous discharge. One way is to try alternate products. Most individuals use a bisacodyl or magic bullet suppository. The bisacodyl has a vegetable coating that must be dissolved in the bowel prior to its working. This can delay the work of the active ingredient that stimulates the bowel. The magic bullet does not have the coating, so it begins working right away. You may find one of these products works better for your needs.
If both products are too stimulating resulting in mucous, the less stimulating glycerin suppository is available. Glycerin suppositories are generally used in children or older adults because it is more gentle. Typically, the higher stimulating suppositories are used in teens and adults but that might not fit your individual need.
Another option is to cut any of the suppositories in half, the long way of the suppository. The long cut leaves the suppository at its manufactured length providing the stimulation to the bowel but with only half of the irritation time. Others might opt for one of the mini enemas (Enemeez or Therevac) that work just in the rectal vault but still must reach the bowel wall to work. They use a different trigger which results in less mucous production.
Overstretching the Bowel and Rectum
Continual dilation (enlarging or widening) of the bowel from lack of a bowel program, excessive gas or slow-moving stool can lead to overstretching of the bowel wall. If this continually occurs, the bowel will not contract back to its typical size. It becomes flaccid, unable to use peristalsis to move stool along rendering it ineffective.
Megacolon and megarectum are dilation of the bowel or rectum. The acute form is a sudden onset, chronic is long standing overexpansion and toxic is when the bowel becomes infected or inflamed in addition to swollen.
Symptoms include bowel distention, nausea and vomiting, bowel obstruction or presence of a hard mass of stool. There can also be fever. Tachycardia or a fast heartbeat can occur. There may be elevated white blood cells present or anemia. Individuals can become dehydrated, have low blood pressure, changes in mental status and electrolyte imbalance. A chronic megacolon can become toxic if the bowel perforates or tears allowing waste or stool into the abdominal cavity.
Testing for megacolon is done by X-ray, CT scan or MRI where the abnormal size of the diameter of the bowel can be seen. Testing for megarectum can be done by digital examination. Treatment for megacolon and megarectum is to remove the impaction and see if the dilation resolves. If caught early this will occur. If the effect in the colon had been present too long or the amount of bowel is too large making the function of the bowel ineffective, surgery might have to be performed to remove a segment of the bowel or a colostomy may be needed to allow for the elimination of waste from the bowel.
Performing the bowel program will reduce your chance of developing this condition. Some people who do develop a mild case will be able to continue their bowel program. Most of the time, the dilation is so slight or affects such a small part of the bowel that people are unaware that it is even present.
Polypharmacy
Taking multiple medications and supplements regularly is polypharmacy. Typically, five medications is the polypharmacy threshold, but some thresholds specify two or more drugs. Medications and supplements can affect the bowel by slowing or speeding. Too slow will lead to constipation, too fast leads to diarrhea. Combination of medications or supplements may affect bowel function differently than use of one medication alone. Be sure to disclose all medications, supplements, holistic drugs, recreational drugs, ointments and lotions to your healthcare professional and pharmacist. They can check drug combinations for unfavorable outcomes. Read the package insert with your medications that will inform you of potential side effects from combinations especially including foods.
Quality of Life
Bowel function issues or concerns about bowel programs is a major factor that affects quality of life for individuals with neurogenic bowel. Difficulties with bowel function can affect all aspects of life including socialization, work, embarrassment, time, eating, enjoyment of food among many other factors.
If your bowel program is affecting any aspect of your life, talk with your healthcare professional. Adjustments to the bowel program can be done to improve it. Changes in bowel programs should be done slowly as it takes a while for the bowel to adjust but progress can be made.
Your mental well-being is critical to success with the bowel program. A therapist can provide strategies to assist you with dealing with potential issues before they become major concerns.
Rectal Issues
Injury to the rectal area can occur from overzealous stool removal, stool that is hard, diarrhea, straining or an unsupported rectal area while sitting on the toilet or commode. The tissue of the rectal area is very fragile. Internal tissue does not welcome dry or rough treatment.
Since the rectal tissue is delicate, hemorrhoids (rectal blood vessels that are overstretched or over-filled with blood) or fissures (a tear in the delicate tissue of the rectal lining) can develop. When tissue becomes damaged, inflammation occurs which is extra blood and body fluid to the area.
Polyps which are bumps of tissue, can also form within the bowel. These might be felt while doing a bowel program but mostly they go unnoticed unless large in size. A colonoscopy should be done every 10 years or less as directed. Many polyps can be removed during this procedure.
Anal abscesses can occur as a pocket of pus anywhere in or around the rectal opening. These form for a variety of reasons from irritation to infection or even for unknown reasons. They can be treated but sometimes anal fistulas can occur when the tract of the abscess remains open with pus draining from it. They are usually treated with antibiotics and wound care. A qualified colorectal surgeon might be needed for surgically clearing the abscess or fistula.
Rectal prolapse occurs when the lower part of the bowel protrudes out of the rectum. It can occur from straining as a technique in bowel emptying in flaccid neurogenic bowel or from sitting with an unsupported rectal area for periods of time. Notice your emptying times to limit time on the toilet or commode to when it is time to empty your bowel and not while you wait. Speak with your healthcare professional about use of straining for toileting. This technique has been removed from current treatment plans, but you might still be using it if you were injured some time ago.
Pilonidal disease is an open area in the skin at the top of the gluteal fold. There may be one, two or sometimes more small openings. An abscess can form under the skin. This is more common in men but either gender can get them. Usually, they are more common in people who are obese or have hair in the area but not always. The cause is unknown. Since they appear over the sacrum, they can be confused with pressure injury as they can grow quite large.
Reflexes
Reflexes can help facilitate bowel evacuation. The gastrocolic reflex occurs when the bowel is stimulated when food or fluid enters the body. It is triggered with every meal but is strongest with breakfast or the morning meal because the gut has slowed (but not stopped) while sleeping at night. This does not mean that the bowel program must performed in the morning. If an evening bowel program is preferred, trigger the gastrocolic reflex by eating a small snack in the evening or even drinking hot water.
Anal stretching for individuals with lower-level injuries can open the rectal sphincters enough for stool to pass through. Check digitally that the rectal vault is empty.
Stool consistency
Stool should be a solid, firm consistency. Not too moist and not too dry. The Bristol Scale, shown above, is a description of stool consistency.
Hard stools are difficult to pass. They can overstretch the bowel as well as become so hard that an impaction develops. An impaction is stool that is blocking the bowel. Typically, no stool will pass but sometimes, liquid stool will pass around the impaction which can be confused with diarrhea. An examination can determine if there is an impaction in the lower bowel. An X-ray is needed to establish if an impaction is higher in the bowel. Manual removal is the method for lower bowel impaction removal. Impactions higher in the bowel might require an enema or oral laxatives.
Vomiting can be the result of indigestion or illness. But it can also be due to an impacted bowel. If stool cannot move downward, it will back up through the digestive tract. Vomiting might be an indication of an impaction. Look at vomit to see if there are any flakes of brown if you suspect an impaction. The flakes or flecks in vomit can be the first sign of the bowel working in reverse. Later, the flakes will be more abundant. Your vomit or breath may smell like stool.
Diarrhea is liquid stool. It occurs when the chyme moves too quickly through the bowel without time for the water and nutrients to be removed. This can occur for a variety of reasons, illness being the most common. Besides gastric distress, stress and anxiety can create an environment in your bowel for diarrhea. If you develop diarrhea, eat bland foods so as not to aggravate the bowel further. An example of a bland diet is the BRAT diet which stand for Bananas, Rice, Apple sauce and Toast. Short term use of electrolyte balanced fluids can help avoid dehydration. Diarrhea can dehydrate you quickly. Medical attention may be needed.
Tone (Spasticity) of the Bowel
Tone or spasticity can occur in any muscle of the body. This includes the bowel. If you have a reflexic (UMN) neurogenic bowel, a brain injury or spinal cord injury from trauma or disease in the cervical or thoracic levels, you may have tone (spasticity) in your body. You can see tone in your legs and arms. Internal tone is not so easy to see. The results of internal body tone are noted through actions. In addition to a slower bowel, tone can prevent chyme or stool from moving forward. Spasticity (tone) can be used to your advantage by use of stimulants (suppository or mini enema) for the bowel program. Gentle digital stimulation can relax the spasticity (tone) of the internal sphincter which allows stool to be expelled from the body. If tone is affecting your bowel program, you can also try muscle relaxing medications, injections, and implants.
Transit Time
The time taken for food to enter your body and leave as stool is called transit time. There are sophisticated tests that can assess the timing of your bowel to work from intake to output. These tests are typically performed in interventional radiology clinics. They involve radiopaque markers that are either administered by IV, ingested by mouth or instilled in the rectum. There is also a test where the individual swallows a pill that contains a tiny camera that will photograph the journey throughout the digestive system. If it is recommended to have one of these tests, it is a good idea to follow through as there will be information gathered that will help you understand the working of your gastrointestinal system as well as to find issues that may be affecting the timing of passage of stool such as an obstruction or other internal issue.
A simple home test yourself will not get all of the helpful information that formal testing will provide, but you can know the average amount of time it takes for your body to move food through your gastrointestinal system from mouth to rectum.
Have a meal where you eat corn. Note the day and time when you eat the corn. An average serving will do. Then no eating corn until it is seen in your stool. Note the day and time you see the corn in your stool. That is your transit time, from when the corn is eaten to when it is expelled. Everyone has a different transit time and it can change depending on what you are doing, the amount and kind of fluid you drink, what you eat, how much you exercise as well as how you feel.
Average transit time for individuals without neurological issues is 12 to 18 hours. Transit time approximates time of passage through the gut. Individuals with spinal cord injury resulting in neurogenic bowel both reflexive and flaccid will have a longer transit time as the passage of food through the bowel can be slower. This is because messages to the brain to increase the muscle contractions in the bowel are not being transmitted or transmitted fully.
You can speed up your bowel transit time by making some lifestyle changes:
- Add activity into your life. Any form of exercise will reflect in the muscles of your abdomen. Activity can be provided through your own body if you are able to do so or passively by someone moving your body for you.
- Standing stretches your muscles in a different direction from sitting and adds weight through your bones. This can help your bowels to function. Standing frames need to be authorized by your payor.
- Movement can be added by doing range of motion exercises or having someone do them to you. Light exercise can be more beneficial to your bowel than heavy exertion. Light movement will increase blood flow to the bowel which aids in movement. Spinal cord injury results in an issue with the nerves but increased blood flow also serves as a milder stimulator.
- Everyday activity can add movement to your body. Be sure to do pressure releases every 15 minutes when up. Manual pressure releases are great but using the tilt button on a power chair also is movement of your body. Rolling in bed for pressure release can add movement to your body. If possible, roll a few extra times. Doing extra movement helps the skin and the bowel.
- In lower-level injuries you may have braces, walk with them. The swinging motion will stimulate the muscles of the abdomen. Walking with braces will increase your activity in your body and in your bowel.
- Participate in sports, aquatic therapy, or anything that you enjoy doing that can add movement which creates activity in your body.
- Sit up during your bowel program. Gravity is your bowel’s friend in that it helps drop the stool out of the bowel. If you do not have a commode chair, ask your healthcare provider to order one that meets your individual needs.
- Adjusting your diet is another way you can try to speed up your bowel through external actions. Give up processed foods and junk foods. That can be difficult so cut down over time. Instead switch to fresh produce and fruit. These foods do not have the fiber already broken down for you, so your body does that in the bowel. Unprocessed foods contain a great deal of natural bulk and fiber. Foods that are rich in fiber include whole grains, beans, nuts, berries, oats, and crunchy vegetables like carrots and celery.
- Pay attention to what you are drinking as well. Try to increase fluid intake slowly if your bladder program allows it. It takes fluid to move stool through your bowel, so you need to be well hydrated. Some drinks dehydrate the body. These include caffeine and alcohol. You can still enjoy these beverages but use in moderation. Avoid sugary and sugar free drinks as these add calories and salt, increase your blood sugar, and do not help with digestion. Foods that are high in fluid content such as soups can add to your fluid intake.
- Have your healthcare provider review your medications for constipation effects. This should include all prescription, over the counter, supplements, recreational or other drugs you may have added along the course of your life. If a medication or combination of medications has the side effect of constipation, ask if there is an alternative. On the other hand, be sure to take stool softeners or other bowel encouraging medications or supplements that work for you. Just be sure to report them on your medication list to ensure you are not compounding your slow bowel when you thought you were helping it.
Pediatric Issues
The pediatric bowel program is critical with infants, children, and adolescents. In infants, diapers are considered culturally acceptable. A neurogenic bowel results from disruption of nerve function. A child of any age with neurogenic bowel requires a bowel program for elimination of stool. A diapered infant or child might have an incontinence, but the bowel is not eliminating all the stool which leads to complications for a lifetime.
Children might discover that others do not do a bowel program. Since it is normal to them, this will be a shock. Keeping the bowel program as normal for them as an individual sets the stage for effective bowel care through life.
Adolescents might have a rebellious period and what could be more powerful than resisting the bowel program. This is a challenging time. Be sure to seek help with dealing with a rebellious teen as the ramifications of not performing the bowel program are great. Bowel incontinence in front of peers is horrific to a teen. It is not something that you want to happen. Making the bowel program normal for the teen is the challenge.
Children typically begin with glycerin suppositories due to the gentle nature of the stimulant. Depending on the age and size of the child, they may be cut in half or even in fourths, the long way, to ensure effectiveness. The adult small finger is used for digital stimulation in infants and small children. Teens move to bisacodyl or magic bullet suppositories as their bodies become more adult. They may find use of a mini enema to be satisfactory.
Transition to independence in doing the bowel program is done anywhere between ages 3 and 5 years. The goal for establishing a functioning bowel program should be prior to going to school to avoid accidents. Start by explaining what you are doing and then have the child join in with gathering supplies, then adding suppository insertion or manual removal and so forth. Plan a stepwise progression to independence. Praise your child for a job well done, perhaps not perfect, but a good attempt. Making the bowel program a natural and normal part of life helps the child to realize this is a natural process.
The older child might not want to participate in their bowel program. Again, it will be up to the parent or caregiver to instill a sense of normalcy about the process. Most will want to complete the bowel program as quickly as possible but taking their time can actually result in less time spent in the overall bowel program process.
Medications for Neurogenic Bowel
There are a large number of medications that can assist with neurogenic bowel programs. Selecting the right medications and supplements requires careful consideration. Adjusting the bowel takes time and patience. Many individuals switch from one product to another or do not get a quick response, so they add more. Take your time to let each product work before adding or switching.
Medication is a common source of constipation. Certain medications have constipation as a side effect. Medications known as constipation culprits are anticholinergics used for bladder treatment, narcotics, calcium channel blockers used to treat high blood pressure, antiseizure medications and antispasmodic medications. Antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs) can lead to diarrhea.
Constipation or diarrhea can develop soon after starting a new medication or may develop after using them for a while so do not overlook them in your bowel function assessment. Check with your healthcare professional about changing to an alternate medication or treat the bowel issue if taking the medication for a limited time.
Commonly used bowel program medications are:
Oral medications
–Stool softeners extract water from the lower bowel to help stool slip through the last section of the bowel and rectum easier. These products contain docusate (examples are Colace, Surfak). Stool softeners are over the counter medications however, they are usually not on the open shelf. They must be requested from the pharmacist if in person or ordered directly online.
–Bulk formers increase the stool size with water from the lower bowel. They are now recommended only for those individuals with areflexic (LMN) neurogenic bowel. These products are psyllium (Metamucil, Fiberall), calcium polycarbophil (Fibercon) and methylcellulose (Citrucel).
–Peristaltic stimulants trigger bowel nerves to increase peristalsis or propelling muscle action. These include senna (Senokot) and senna with docusate (Peri-Colace with senna).
-Many other medications for neurogenic bowel are options depending on your individual bowel program plan. These include polyethylene glycol (MiraLAX), milk of magnesia, magnesium citrate, lactulose, and sorbitol.
Rectal Medications
– Contact irritants are suppositories and mini enemas. Stimulants must be inserted next to the bowel wall to stimulate the bowel to function. Removal of stool might need to be done to achieve placement for the stimulant to work.
The least harsh is a glycerin suppository which irritates the lower bowel for evacuation. It is used for pediatric and often geriatric patients as it is the least stimulating.
The next level of suppository is the bisacodyl (Dulcolax) or Magic Bullet which stimulate nerve endings when in contact with the bowel wall. Bisacodyl has a vegetable coating which allows a bit more time to melt. Also made from bisacodyl is the Magic Bullet suppository without the vegetable coating that has a quicker melting time. It is a bit of trial and error to establish your personal preferences.
Mini enema (Enemeez or Therevac) is a small volume enema that stimulates water absorption in the stool and nerve function within the rectal vault. Enemeez Plus includes an anesthetic if pain or AD are issues. These are alternatives to suppositories. Like a suppository, the mini enema must be placed next to the bowel to work so manual stool removal may be necessary. Digital stimulation still needs to be performed. Follow delivery instructions carefully to avoid a tear in the bowel tissue.
–Lubricant is an over-the-counter substance that is used consistently in the bowel program. This is applied to the non-latex gloved finger for insertion of the suppository and to perform digital stimulation. The lubricant should be water soluble such as K-Y jelly or ASTROGLIDE. Some lubricants are less ‘drippy’ but more expensive. Avoid those lubricants that might be cheaper but not water soluble such as petroleum jelly as they will not dissolve, and you will be left with a goopy mess. Drop the lubricant on to the gloved finger or where you are using it being careful not to touch the multi-use tube to anything to avoid contamination of the rest of the lubricant.
–Anesthetic ointments Additional medications may be needed for specific circumstances such as with sensation, pain, presence of hemorrhoids or autonomic dysreflexia (AD). Some individuals will use a numbing ointment such lidocaine rectal ointment. This is inserted five to ten minutes prior to starting the bowel program.
Medications Not or No Longer Recommended for Neurogenic Bowel
Many of these products have been recommended to individuals with neurogenic bowel over the years. You may find you rely on one or more of these. New guidelines have clarified their use especially in spinal cord injury. If you find you are using these techniques or products, even if they are working well for you, check with your healthcare professional to see if you should continue or change to another product.
-Bulk fiber laxatives are fiber building additives for the stool for individuals with reflexic (UMN) neurogenic bowel. The idea was to build bulk in the stool to make passage through the intestines quicker, softer, and with bulk for the intestines to pass stool along. However, new guidelines suggest that this is counteractive because individuals with reflexic (UMN) neurogenic bowel cannot take in the amount of fluid needed to stimulate the bulk fiber to work. Without the recommended fluid, the bulk fiber becomes extremely hard in the stool which creates impaction, stool that is difficult to pass, and stool that has rough edges which can tear or cut the bowel or anus.
Individuals who monitor their fluid intake or have health conditions that limit fluid intake such as heart conditions or extreme edema cannot take in the recommended fluid amounts. Others have not been educated about the eight ounces of fluid needed. They may have even received a low fluid amount in a health care setting which makes individuals feel that the total amount of fluid is not required.
If you have an areflexic (LMN) neurogenic bowel or other bowel condition and are taking a bulk fiber laxative with the proper amount of fluid that is providing moist assistance to your bowel program, be sure you are using products with no added sugar. A secondary complication of spinal cord injury and other neurological disorders is adult-onset diabetes. The extra sugar can add to your risk of developing or affecting diabetes.
Check with your health professional to see if you should still be taking a bulk fiber laxative product. You may find it is working against your bowel program goals or that another product will better suit your needs.
-Enemas are most generally saved for serious situations such as impaction as they tend to wipe out the natural health bacterial flora of the bowel and do not provide the normal bowel peristalsis action. Enemas can damage fine fibers in the bowel that move the stool forward and out.
-Laxatives are another group of bowel preparation products that are not recommended for a bowel program. The unpredictability of the product, washing away of the healthy bacterial flora, and reduction in bowel peristalsis make these products too unpredictable for use. Individuals can become reliant on laxatives for bowel movements regardless of their health condition. When this occurs, a bowel movement will not happen without the laxative which can make a bowel movement even more difficult to accomplish. What seems to be helping in the short term will lead to serious complications in the long term.
-Natural products from health and vitamin stores are felt to be strongly essential by many individuals. Be sure you discuss each product with your healthcare professional. Sometimes a natural product is actually a laxative, diuretic or can interfere with other medications. Many of the clerks in the health store are knowledgeable about their products but some have a limited knowledge about health needs and are not versed in neurogenic bowel issues. Be sure you speak with an informed healthcare professional prior to embarking on a bowel regimen that may not be to your advantage.
-Probiotics have been identified as having some health disadvantages. Therefore, they should not be recommended on an ongoing basis. Recommendations are for use with antibiotic associated diarrhea and Clostridium difficile (C. diff)-associated diarrhea (CDAD).
Surgical Options
Surgical options may be considered for individuals who face challenges with neurogenic bowel programs. Some individuals think that a surgical alternative would be a better choice because they do not like the idea of performing the bowel program or it takes too much time or any of a variety of valid reasons. The goal of the bowel program is to have your bowel function in its natural way. Surgical decisions should be carefully considered.
Malone antegrade continence enema (MACE)
MACE is a surgical procedure where the appendix is connected to a permanent opening to the abdominal wall. A catheter is used to irrigate the bowel and rectum for waste removal. Advantages include no bag for collection and little leakage. Complications can include stomal stenosis, stomal site infection, possible leakage through the stoma, and difficulty with stomal catheterization.
Not many are aware of this procedure. It has a high success rate with improvement in quality of life and reduction of autonomic dysreflexia (AD) episodes.
Colostomy
A colostomy is a surgically created artificial opening in the abdomen where the large intestine of the bowel is then connected. Stool is excreted through the opening. A bag is taped to the skin around the opening to collect the stool.
Some thinking points about colostomy include the following:
As with any surgery, colostomy surgery can be dangerous for an individual with neurological issues especially due to respiratory complications. Be sure to evaluate the risks vs. benefits before thinking about any dramatic procedure.
It can be more difficult to maintain a colostomy than to perform a bowel program. Changing bags, bags falling off or bursting, irrigation of the colostomy are just a few of the issues that can arise.
Colostomy bags can be difficult to secure to the abdomen. The brochure makes bag use look easy, but colostomy bags work best on a muscular abdomen. Securing a colostomy bag on the typical abdomen can be a challenge.
Not all health payors will finance the supplies and care for a colostomy which can be expensive. Investigate costs and payor resources prior to making this financial responsibility.
Elective colostomy allows placement options. Closer to the end of the large intestines will result in expulsion of stool-like contents. The farther up the large intestine, the looser the stool will be. Individuals have preferences about colostomy location by stool type and convenience.
Individuals Involved with Treatment of Neurogenic Bowel
Many individuals will assist you to create an effective bowel management program.
A Physiatrist is a physician who has advanced education in physical medicine and rehabilitation needs. Some have specialty areas in brain injury or spinal cord injury, but all will be able to assess and prescribe rehabilitation techniques as well as to problem solve issues.
Rehabilitation nurses provide instruction and care of individuals with neurogenic bowel. They have an extensive knowledge of how to perform the bowel programs as well as problem solving.
A Gastroenterologist is a physician who will be able to assist with testing, diagnosis, and treatment of neurogenic bowel as well as other issues that can arise in the gastrointestinal (GI) system.
A Gastrointestinal (GI) surgeon specializes in surgical procedures of the GI system. This can include surgery for hemorrhoids, fissures, fistulas, rectal prolapse, MACE and colostomy.
A Registered Dietitian assists with education about planning food choices that will make your bowel management a success.
The Physical Therapist provides therapy and instruction for toileting transfers, muscle strengthening, electrostimulation, and movement.
The Occupational Therapist can assist with bowel management program design. They are resources for adaptive equipment such as suppository insertion, digital stimulation, electrostimulation, and commodes.
Wound care specialists are Registered Nurses that provide education about ostomy care.
Dentists keep your teeth and mouth in good condition to ensure an effective start to the digestive process.
Issues and Treatments of the Digestive Process
Individuals with neurogenic bowel are not exempt from common bowel issues. These bowel concerns may impact your health in addition to the effects of neurogenic bowel.
Digestion and bowel function rely on the entire digestive system or gastrointestinal (GI) tract working well. Any issue at any point in the processing of food and fluid can affect bowel management. Therefore, it is important to review all phases of digestion to create an environment in your body to improve bowel function. People often just think about the output of the bowel as affecting function, but a disruption anywhere along the GI path can affect output.
Mouth
Be sure you are smelling, seeing, and tasting food. If any or multiple senses are not functioning correctly, your enjoyment of food will be reduced. Your healthcare professional can easily test your senses in a medical office by assessing your cranial nerve function. If there is a concern with any of your senses, you may be referred for further testing using MRI or CT scans to look for the source.
Teeth are critical to be able to chew food. Chewing is the first step in breaking food down so it can be further manipulated by the stomach. Chewing foods into smaller particles allows more surface area for saliva and stomach acids to create small particles for digestion. The less chewing, the more work is placed on the stomach or even the small intestine to extract nutrients from food. Too large of particles will not be able to be extracted and can pass through the bowel still intact.
Good dental care is important to eating. This can prevent loss of teeth, dental caries (cavities) and sores in the mouth. Be sure to do your part to keep your mouth clean and free from food particles which can lead to pneumonia if inhaled or contribute to dental decay if left in your teeth. Adaptive equipment can assist you with your dental needs such as handcuffs for holding toothbrushes, dental floss on a toothbrush style handle and toothbrushes that attach to suction machines.
Swallowing should be assessed if there is an issue prior to putting food or fluid into the mouth. A swallow study may be done to ensure swallowing is safe and that there is no leaking of food or fluid into the lungs. Simple swallow assessments can be performed at the bedside, but more definitive studies are done in healthcare settings by educated professionals using multiple textures and fluorescence (X-ray) to view your internal swallowing ability.
Mouth sores or discomfort can lead to pain which makes individuals slow or even stop eating and drinking. They can reduce the taste of food or even make it taste bad. There are several conditions that affect the mouth and thus the ability to eat. Most of mouth symptoms are sores, blisters, red spots, pain and swelling. Treatment is based on the cause. These conditions include:
- Allergic reaction
- Canker sores
- Angioedema (face and body swelling)
- Medication reaction or side effect
- Coxsackie virus infection (hand, foot, and mouth disease)
- Anemia, iron deficiency
- Mouth (oral) cancer
- Poison ivy, oak, and sumac
- Scarlet fever
- Ulcerative colitis
- Cellulitis (infection of the cells)
- Insect bites/sting
- Salivary duct obstruction (sialolithiasis)
- Pemphigus (chronic blisters)
- Erythema multiforme (autoimmune skin disease)
- Drug allergy
- Esophagitis (infection of the esophagus)
- Burn (heat or fire)
- Chemical burns
- Crohn’s disease
- Thermal burn of mouth or tongue
Stomach
Stomach contents can back up into the esophagus which can irritate and stretch esophageal tissue. This can be unnoticeable or with symptoms of coughing or a burning sensation typically called heartburn. If this is progressive, gastro esophageal reflux disease (GERD) is diagnosed. Over the counter and prescription medication are usually suggested. Sleeping with the head of the bed elevated or the head of the bedframe on risers may also help. Continued reflux should be examined to ensure the esophagus is free from erosion, ulcers, and cancer.
Upset stomach is called dyspepsia. If you have an intermittent or continual dyspepsia, you will need to be assessed for issues that can be affecting the lining of your stomach which would slow the digestive process. Stomach lining issues can lead to slow digestion or scarring of the muscle tissue. These concerns may include gastric ulcer (stomach ulcer), peptic ulcer disease, gastritis (inflammation of the stomach), stomach cancer, gastric varices (enlarged veins), or stomach bleeding. Gastritis is an inflammation of the stomach that can be from many causes–one is from a bacterium, H. pylori. Medications to reduce stomach acid production or to treat infections are typically prescribed. Occasionally, surgical repair of ulcers is needed.
Gastroparesis is a condition of the stomach where gastric emptying is delayed. Issues that can cause gastroparesis are as a result of paralysis, nerve damage from diabetes or other conditions that impair the stomach’s muscle contractions. Medication can help increase stomach actions.
Assessments of the stomach include:
Upper endoscopy (esophagogastroduodenoscopy or EGD): A tube that is passed through the mouth into the esophagus, stomach, and duodenum to visually examine the tissue. PH testing can be done to assess acid levels for GERD. A biopsy of the esophagus or stomach can be made at this time.
Barium swallow: A solution that can be used with X-ray is ingested followed by images of the upper digestive system to look for issues or concerns like ulcers or other problems.
Upper GI series, Computed Tomography (CT scan) or Magnetic Resonance Imaging (MRI): are types of imaging studies to view the body’s contents.
Gastric emptying study which assesses the length of time for food to pass through the stomach.
H. pylori test: a blood or stool test can indicate the presence of this infection.
Intestines
Issues in the intestines are numerous. Any concern with the intestines can affect movement of chyme through the bowel either too quickly or too slowly. Common bowel issues are:
- Bleeding (hemorrhage): can be slow or gushing
- Cancer or tumor
- Celiac disease: reaction to gluten (a protein) which leads to absorption issues in the small intestine
- Colitis: inflammation of the intestine
- Constipation: dry stool
- Diarrhea: watery stool
- Diverticulosis or Diverticulitis: weak areas in the intestine wall which can become inflamed or infected.
- Inflammatory bowel disease/Irritable bowel syndrome (IBS): Crohn’s disease or ulcerative colitis
- Intestinal obstruction: a blocked, twisted or malfunction in part or both intestines
- Intussusception: the small intestine collapses into itself, mostly in children
- Polyps: growths in the intestines
- Salmonellosis/Shigellosis/Traveler’s Diarrhea: bacterial infections
- Stomach flu (enteritis): from viruses, bacteria, or parasites
Many treatments for the intestines are provided by use of over the counter and prescription medications to speed or slow the bowel. Antibiotics are given for infection. Treatment of bowel conditions depend on extent of the issue. They are often done during a colonoscopy procedure or with surgery. Assessments of the intestines include:
Colonoscopy is a commonly performed test of the intestines. A tube is inserted into the rectum. The entire colon can be visually inspected. Biopsies can be done. Polyps and small tumors can be removed. X-rays can be taken. If just the lower colon is viewed, the test is called a sigmoidoscopy. Prior to colonoscopy testing, an extensive bowel prep or cleanse is performed. Individuals with spinal cord injury may be able to be admitted to the hospital for the bowel prep. Check with your payor.
Fecal occult blood testing is a test for blood by examining a smear of stool.
Rectum
There are several issues that can occur in and around the rectum as this is the last section of the digestive tract within the body.
- Abscess: a collection of pus at or around the rectal opening
- Bleeding: rectal bleeding can be from anywhere higher in the digestive tract or at the rectum
- Cancer
- Hemorrhoids: enlarged veins within the rectum or at the rectal opening
- Fissures and fistulas: fissures are cracks in the bowel membrane, fistulas are tracts from the bowel to other parts of the bowel or other body organs
- Pilonidal disease: is an open area in the skin at the top of the gluteal fold
- Rectal prolapse: the internal rectum protrudes out of the anus
Assessment and treatment of rectal issues is done by physical assessment through visualization of the rectum, a digital examination, an anoscope or a sigmoidoscopy. Treatment can include antibiotics for infection, medical treatment, or surgical intervention. It is recommended that individuals with neurological issues who require advanced treatment for hemorrhoids have conservative procedures rather than surgical excision.
Research
Better understanding of how the digestive system works specifically in nerve related issues of the bowel is being heavily researched. This includes bowel function, nervous system function, drug responses, and improvements in bowel management procedures. Quality of life due to alterations in bowel function drives many of these studies to improve life satisfaction for individuals with neurogenic bowel.
Research has enhanced care for individuals with neurological injury. If muscles are stimulated with electrical medical devices, these are used to enhance function and recovery. This treatment is used for individuals with reflexic (UMN) injury. For individuals with areflexic (LMN) injury, functional electrical stimulation can be used at the zone of transition to strengthen muscles which results in increased function and with peripheral nerve stimulation especially for bladder and bowel control and sexual function in males.
Implants of functional electrical devices are available in research settings but soon to be available in general. Opportunities for this type of treatment will become more common as progress is occurring rapidly. This will create a huge opportunity for reduction of secondary complications of spinal cord injury as well as enhancing function and even recovery. This includes both reflexic (UMN) and areflexic (LMN) injuries. Significantly, nerve rerouting procedures to peripheral nerves to improve function and avoid complications are available.
Many research studies are being conducted to better understand neurotransmitters especially glutamate and acetylcholine, scaffolding which allows transplanted nervous tissue or stem cells to remain in the area of neurologic injury as well as disease specific studies. This is a time of major leaps in neurological research and treatment. Not as quickly as we would all be desiring but in scientific time, a huge leap.
Researchers are especially keen to understand fetal and early development to be able to harness the rapid growth of the nervous system to treatment options. This is another way science is seeking to improve the lives of individuals with neurological issues.
Facts and Figures
The number of individuals with neurogenic bowel dysfunction is unknown as there is no central collection repository. Estimates in the overall population are between 1% to 25% depending on definitions and terms used.
Estimates of neurogenic bowel by disease or injury varies by source. Many common diagnoses do not have reports of prevalence of neurogenic bowel. Some diagnoses with averages of reports of neurogenic bowel are:
- Stroke 15%
- Spinal cord injury 80%
- Multiple Sclerosis 60%
- Myelomeningocele 68%
- Parkinson’s Disease 47-75%
Commonly reported symptoms of neurogenic bowel after spinal cord injury include:
- Constipation 32-56%
- Bowel incontinence 27-86%
- Digital stimulation required 66%
- Manual evacuation 66%
- Abdominal distention and discomfort 22% to 33%
- Hemorrhoids 31% to 36%
- Average time for each defecation: more than 30 minutes–25%, more than an hour– 9%
Bowel maintenance
Adaptive Tools for Independence: Bowel Management Tools
Bowel care is very personal! This video highlights how a person with a spinal cord injury at C7 uses adaptive equipment to perform his own bowel cares. These items can be found online or with the help of an occupational therapist.
This video, created by Christopher & Dana Reeve Foundation and Craig Hospital, highlights functional tools or adaptive equipment available for people with hand weakness who would like to gain more independence in their daily activities.
Resources
If you are looking for more information about bowel management or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 9:00 am to 8:00 pm ET.
Additionally, the Reeve Foundation maintains a bowel management fact sheet with additional resources from trusted Reeve Foundation sources. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
We encourage you to reach out to support groups and organizations, including associations which feature news, research, resources, national network of support groups, clinics, and specialty hospitals.
Neurogenic Bowel Care Guidelines and Fact Sheets
Christopher & Dana Reeve Foundation. Bowel Management booklet
Paralyzed Veterans of America (PVA). Neurogenic Bowel: What You Should Know: A Guide for People with Spinal Cord Injury. see Consumer Guidelines
Spina Bifida Association. Guidelines for the Care of People with Spina Bifida
National Institute of Neurological Disorders and Stroke: Motor Neuron Diseases Fact Sheet
Further Reading
Ambartsumyan L, Rodriguez L. Bowel management in children with spina bifida. J Pediatr Rehabil Med. 2018;11(4):293-301. doi: 10.3233/PRM-170533. PMID: 30507592.
Awad RA. Neurogenic bowel dysfunction in patients with spinal cord injury, myelomeningocele, multiple sclerosis and Parkinson’s disease. World J Gastroenterol. 2011 Dec 14;17(46):5035-48. doi: 10.3748/wjg.v17.i46.5035. PMID: 22171138; PMCID: PMC3235587.
Bernardi M, Fedullo AL, Bernardi E, Munzi D, Peluso I, Myers J, Lista FR, Sciarra T. Diet in neurogenic bowel management: A viewpoint on spinal cord injury. World J Gastroenterol. 2020 May 28;26(20):2479-2497. doi: 10.3748/wjg.v26.i20.2479. PMID: 32523306; PMCID: PMC7265150.
Chen G, Liao L, Wang Y, Ying X. Effect of sacral neuromodulation on bowel dysfunction in patients with neurogenic bladder. Colorectal Dis. 2020 Jul 18. doi: 10.1111/codi.15273. Epub ahead of print. PMID: 32681678.
Coggrave M, Norton C. Neurogenic bowel. Handb Clin Neurol. 2013;110:221-8. doi: 10.1016/B978-0-444-52901-5.00018-6. PMID: 23312643.
Coggrave M, Norton C, Cody JD. Management of faecal incontinence and constipation in adults with central neurological diseases. Cochrane Database Syst Rev. 2014 Jan 13;(1):CD002115. doi: 10.1002/14651858.CD002115.pub5. PMID: 24420006.
Cotterill N, Madersbacher H, Wyndaele JJ, Apostolidis A, Drake MJ, Gajewski J, Heesakkers J, Panicker J, Radziszewski P, Sakakibara R, Sievert KD, Hamid R, Kessler TM, Emmanuel A. Neurogenic bowel dysfunction: Clinical management recommendations of the Neurologic Incontinence Committee of the Fifth International Consultation on Incontinence 2013. Neurourol Urodyn. 2018 Jan;37(1):46-53. doi: 10.1002/nau.23289. Epub 2017 Jun 22. PMID: 28640977.
Deng Y, Dong Y, Liu Y, Zhang Q, Guan X, Chen X, Li M, Xu L, Yang C. A systematic review of clinical studies on electrical stimulation therapy for patients with neurogenic bowel dysfunction after spinal cord injury. Medicine (Baltimore). 2018 Oct;97(41):e12778. doi: 10.1097/MD.0000000000012778. PMID: 30313096; PMCID: PMC6203582.
Doherty JG, Burns AS, O’Ferrall DM, Ditunno JF Jr. Prevalence of upper motor neuron vs lower motor neuron lesions in complete lower thoracic and lumbar spinal cord injuries. J Spinal Cord Med. 2002 Winter;25(4):289-92. doi: 10.1080/10790268.2002.11753630. PMID: 12482171.
Elmelund M, Klarskov N, Biering-Sørensen F. Fecal incontinence and neurogenic bowel dysfunction in women with traumatic and nontraumatic spinal cord injury. Dis Colon Rectum. 2019 Sep;62(9):1095-1104. doi: 10.1097/DCR.0000000000001446. PMID: 31318774.
Emmanuel A. Neurogenic bowel dysfunction. F1000Res. 2019;8:F1000 Faculty Rev-1800. Published 2019 Oct 28. doi:10.12688/f1000research.20529.1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6820819/
Furness JB, Callaghan BP, Rivera LR, Cho HJ. The enteric nervous system and gastrointestinal innervation: integrated local and central control. Adv Exp Med Biol. 2014;817:39-71. doi: 10.1007/978-1-4939-0897-4_3. PMID: 24997029.
Gater DR. Neurogenic bowel and bladder evaluation strategies in spinal cord injury: New directions. J Spinal Cord Med. 2020 Mar;43(2):139-140. doi: 10.1080/10790268.2020.1718469. PMID: 32105585; PMCID: PMC7054921.
Gor RA, Katorski JR, Elliott SP. Medical and surgical management of neurogenic bowel. Curr Opin Urol. 2016 Jul;26(4):369-75. doi: 10.1097/MOU.0000000000000299. PMID: 27152922.
Hou S, Rabchevsky AG. Autonomic consequences of spinal cord injury. Compr Physiol. 2014 Oct;4(4):1419-53. doi: 10.1002/cphy.c130045. PMID: 25428850.
Hultling C. Neurogenic bowel management using transanal irrigation by persons with spinal cord injury. Phys Med Rehabil Clin N Am. 2020 Aug;31(3):305-318. doi: 10.1016/j.pmr.2020.04.003. Epub 2020 Jun 2. PMID: 32624096.
Kairaluoma MV. Toiminnallinen ulostamisvaikeusoireyhtymä [Functional obstructed defecation syndrome]. Duodecim. 2009;125(2):221-5. Finnish. PMID: 19341037.
Kelly MS, Wiener JS, Liu T, Patel P, Castillo H, Castillo J, Dicianno BE, Jasien J, Peterson P, Routh JC, Sawin K, Sherburne E, Smith K, Taha A, Worley G. Neurogenic bowel treatments and continence outcomes in children and adults with myelomeningocele. J Pediatr Rehabil Med. 2020;13(4):685-693. doi: 10.3233/PRM-190667. PMID: 33325404.
Krassioukov A, Eng JJ, Claxton G, Sakakibara BM, Shum S. Neurogenic bowel management after spinal cord injury: a systematic review of the evidence. Spinal Cord. 2010 Oct;48(10):718-33. doi: 10.1038/sc.2010.14. Epub 2010 Mar 9. PMID: 20212501; PMCID: PMC3118252.
Musco S, Bazzocchi G, Martellucci J, Amato MP, Manassero A, Putignano D, Lopatriello S, Cafiero D, Paoloni F, Del Popolo G. Treatments in neurogenic bowel dysfunctions: evidence reviews and clinical recommendations in adults. Eur J Phys Rehabil Med. 2020 Dec;56(6):741-755. doi: 10.23736/S1973-9087.20.06412-6. Epub 2020 Sep 16. PMID: 32935955.
Nelson MES, Orr M. Digital rectal stimulation as an intervention in persons with spinal cord injury and upper motor neuron neurogenic bowel. An evidenced-based systematic review of the literature. J Spinal Cord Med. 2019 Dec 6:1-8. doi: 10.1080/10790268.2019.1696077. Epub ahead of print. PMID: 31809250.
Nielsen SD, Faaborg PM, Finnerup NB, Christensen P, Krogh K. Ageing with neurogenic bowel dysfunction. Spinal Cord. 2017 Aug;55(8):769-773. doi: 10.1038/sc.2017.22. Epub 2017 Mar 14. PMID: 28290468.
Pardee C, Bricker D, Rundquist J, MacRae C, Tebben C. Characteristics of neurogenic bowel in spinal cord injury and perceived quality of life. Rehabil Nurs. 2012 May-Jun;37(3):128-35. doi: 10.1002/RNJ.00024. PMID: 22549630.
Powell A, Davidson L. Pediatric spinal cord injury: a review by organ system. Phys Med Rehabil Clin N Am. 2015 Feb;26(1):109-32. doi: 10.1016/j.pmr.2014.09.002. PMID: 25479784.
Previnaire JG. The importance of the bulbocavernosus reflex. Spinal Cord Ser Cases. 2018 Jan 10;4:2. doi: 10.1038/s41394-017-0012-0. PMID: 29423307; PMCID: PMC5798690.
Preziosi G, Gordon-Dixon A, Emmanuel A. Neurogenic bowel dysfunction in patients with multiple sclerosis: prevalence, impact, and management strategies. Degener Neurol Neuromuscul Dis. 2018 Dec 6;8:79-90. doi: 10.2147/DNND.S138835. PMID: 30584387; PMCID: PMC6287516.
Qi Z, Middleton JW, Malcolm A. Bowel dysfunction in spinal cord injury. Curr Gastroenterol Rep. 2018 Aug 29;20(10):47. doi: 10.1007/s11894-018-0655-4. PMID: 30159690.
Sasaki H, Kawamura N, Dyck PJ, Dyck PJB, Kihara M, Low PA. Spectrum of diabetic neuropathies. Diabetol Int. 2020 Jan 8;11(2):87-96. doi: 10.1007/s13340-019-00424-7. PMID: 32206478; PMCID: PMC7082443.
Stern M. Neurogenic bowel and bladder in the older adult. Clin Geriatr Med. 2006 May;22(2):311-30; ix. doi: 10.1016/j.cger.2005.12.014. PMID: 16627081.
Stoffel JT, Van der Aa F, Wittmann D, Yande S, Elliott S. Neurogenic bowel management for the adult spinal cord injury patient. World J Urol. 2018 Oct;36(10):1587-1592. doi: 10.1007/s00345-018-2388-2. Epub 2018 Jun 27. PMID: 29951791.
Tulsky DS, Kisala PA, Victorson D, Tate DG, Heinemann AW, Charlifue S, Kirshblum SC, Fyffe D, Gershon R, Spungen AM, Bombardier CH, Dyson-Hudson TA, Amtmann D, Kalpakjian CZ, Choi SW, Jette AM, Forchheimer M, Cella D. Overview of the Spinal Cord Injury–Quality of Life (SCI-QOL) measurement system. J Spinal Cord Med. 2015 May;38(3):257-69. doi: 10.1179/2045772315Y.0000000023. PMID: 26010962; PMCID: PMC4445018.
Yeung HY, Iyer P, Pryor J, Nicholson M. Dietary management of neurogenic bowel in adults with spinal cord injury: an integrative review of literature. Disabil Rehabil. 2019 Aug 15:1-12. doi: 10.1080/09638288.2019.1652702. Epub ahead of print. PMID: 31415185.
Yim SY, Yoon SH, Lee IY, Rah EW, Moon HW. A comparison of bowel care patterns in patients with spinal cord injury: upper motor neuron bowel vs lower motor neuron bowel. Spinal Cord. 2001 Apr;39(4):204-7. doi: 10.1038/sj.sc.3101131. PMID: 11420735.
Zhang Y, Xia X, Zhuang X. Effect of quantitative assessment-based nursing intervention on the bowel function and life quality of patients with neurogenic bowel dysfunction after spinal cord injury. J Clin Nurs. 2018 Mar;27(5-6):e1146-e1151. doi: 10.1111/jocn.14198. PMID: 29193471.
Zidek K, Srinivasan R. Rehabilitation of a child with a spinal cord injury. Semin Pediatr Neurol. 2003 Jun;10(2):140-50. doi: 10.1016/s1071-9091(03)00022-6. PMID: 14572150.