Spina Bifida
Shortly after conception, when cells are just beginning to develop, the brain and the spinal cord are formed from a structure called the embryonic neural tube. The neural tube folds and closes at the third and fourth weeks of pregnancy. Rarely, a part of the neural tube does not fully fold and close which is called a neural tube defect. This can happen anywhere in the area of the formation of the brain and spine. When the neural tube does not fully develop in the brain, anencephaly (part of the brain and skull are not formed) or encephalocele (out pouching at the skull) occurs. An opening in the spine occurs if the spinal cord section of the neural tube does not fold and close completely. The vertebral bone column does not form in the area. This is diagnosed as spina bifida.
Spina bifida is typically identified before or at birth. There are occurrences of diagnosis in adulthood. This is typically in spina bifida occulta where there are no symptoms. However, as people age the body might not accommodate as in youth leading to issues where spina bifida is typically discovered and diagnosed.
Why spina bifida occurs is not fully understood. There is evidence that it is due in part to a lack of folic acid in the mother’s diet. In the month prior to conception and in the first three months of pregnancy, additional folic acid should be taken to assist with the closure of the neural tube. Folic acid is a nutrient found in foods however, a typical diet does not contain the needed amounts and it is difficult to achieve. Therefore, the Centers for Disease Control and Prevention (CDC) recommends women take 400 mcg of folic acid supplement daily but if pregnancy is considered, this amount should be raised to 4000 mcg.
Taking prenatal vitamins when considering pregnancy is important as other vitamin deficiencies may contribute to spina bifida. Other prevention to begin before and during pregnancy include eating a balanced diet, controlling diseases such as diabetes and obesity, avoiding overheating your body by not using hot tubs, saunas, and controlling fever. These are general considerations. Specific evidence of these causes leading to spina bifida has not yet been noted.
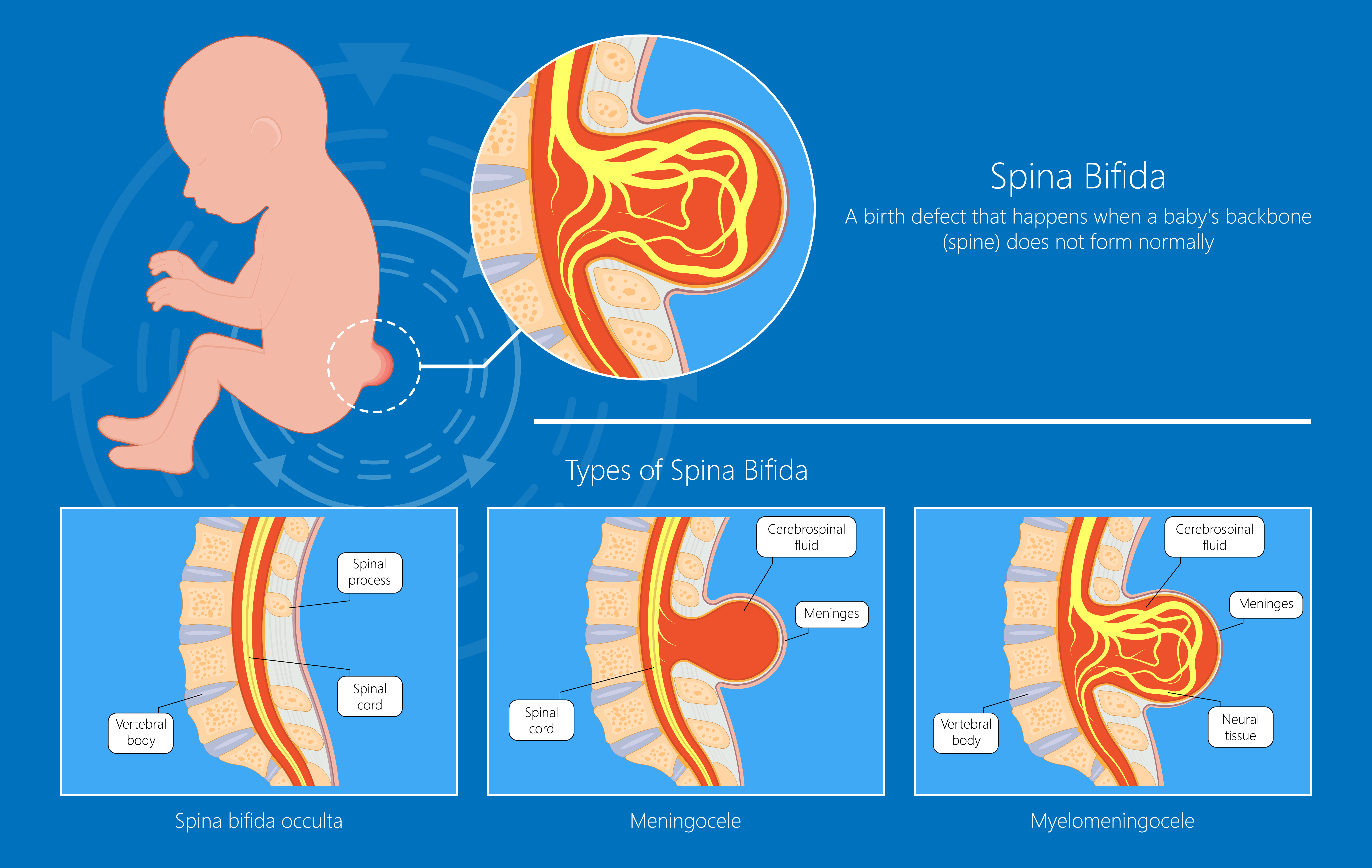
There are types of spina bifida that are classified by the specifics of the injury.
Spina Bifida Occulta is a mild form of spina bifida where the spine is open, but the spinal cord is not out of the usual placement. There is generally no pouch on the back. Very minimal, if any changes, in function and sensation occur. An individual may not realize they even have this diagnosis. The skin of the back may have no changes, a dimple over the area or a tuft of hair.
Meningocele diagnosis is made when there is a pouch of cerebral spinal fluid (the liquid that cushions the brain and spine) protruding on the back over the spine. The spinal cord nerves do not extend into this pouch. There may be some mild changes in function.
Myelomeningocele diagnosis is a pouch on the back that includes cerebral spinal fluid and part of the spinal cord and nerves. The individual typically has changes in functional abilities such as walking, toileting, and sensation. There are associated diagnoses that are found with myelomeningocele that include hydrocephalus (too much cerebral spinal fluid surrounding the brain), which can result in learning disabilities, coordination problems, visual problems and epilepsy.
Conditions Associated with Spina Bifida
Some health conditions might occur in higher incidence with differing types of spina bifida. These concerns may be in conjunction with the neural tube issue from pulling, swelling, inflammation, tethered cord or other consequences that are not fully understood. Not everyone with spina bifida has these conditions but often they coincide. This list can be overwhelming. Most individuals with spina bifida do not have all these possible conditions.
Attention and Learning Difficulty Children, especially with hydrocephalus may have learning difficulty. This can be in understanding, conceptualization, motor planning or other issues. An evaluation by a neuropsychologist using developmentally appropriate testing can help pinpoint specific needs so teaching techniques and adaptations can be implemented. An Individual Education Plan (IEP) will be created by school personnel with input from healthcare providers and parents or guardians. This plan is then followed to establish a conducive learning environment. As a parent or guardian, you will want to carefully review the document before approving it to ensure your child’s needs are met in the most effective manner.
Bladder Function As a result of spina bifida, bladder function can be neurogenic (issues with nerve control), with urinary retention, incomplete emptying or a combination. The individual might spontaneously urinate but not completely empty the bladder leading to repeated infections and kidney failure. Because babies wear diapers, bladder function can be misinterpreted. An assessment of how the bladder functions will be completed either by an X-ray, ultrasound, CT or MRI with contrast to visualize bladder and kidney function, a catheterization to check the amount of urine left in the bladder after emptying called a post void residual, a bedside bladder scan or ultrasound, or a urodynamics study (a test that assesses the entire urinary system). A program of intermittent catheterization can control effective bladder emptying.
Protection of kidney function is extremely important in keeping your child healthy into the future. Urine that backs up from the bladder (a urine storage organ) to the kidneys (a non-storage organ) can damage delicate kidney tissue causing kidney failure. Kidney damage is more prevalent in people with spina bifida. Further information about bladder function and treatment is available from the National Institute of Diabetes and Digestive and Kidney Diseases.
Bowel Function Neurogenic bowel function, incontinence or incomplete emptying will be assessed. Because babies use diapers, neurogenic bowel can be overlooked leading to bowel issues later in life. Successful elimination can be achieved through implementation of a bowel program. Infants typically begin with a glycerin suppository cut in quarters lengthwise to stimulate a complete bowel movement and is advanced as they grow. Dietary inclusion of roughage, adding bulk to the stool and fluid can assist with bowel elimination. Medication such as liquid stool softeners also assist with the bowel program.
Depression For some individuals with spina bifida as with all individuals with chronic healthcare concerns, depression can occur in higher incidences. Working with a psychologist or counselor can help identify issues as well as provide strategies for the individual and family.
Epilepsy and Seizures Some individuals develop seizures or epilepsy mostly due to effects of spina bifida, hydrocephalus and brain trauma or injury. Tethering of the spinal cord can create tension of the brain before release but with the effect of seizure development. There are a variety of reasons why epilepsy or seizures can develop in individuals with spina bifida. Medications are used to help control seizures.
Hip Displacement As an infant, the hips will need to be assessed for correct placement and movement. Due to muscle weakness, the hips are susceptible to displacement both at birth and in future development. Strengthening exercises, therapeutic intervention and adaptive equipment will be provided. Additional therapy will be needed as the child grows and becomes more independent.
Hydrocephalus This condition is a collection of an overabundance of cerebral spinal fluid within and surrounding the brain that is more than is typical. It may be present before or develop after birth. When there is extra fluid in the enclosed, rigid skull, pressure builds and can damage the delicate nerve tissue. It is corrected by placement of a shunt (tube) that drains the extra fluid into the stomach or abdomen for removal by the body. The shunt will have a coil in the abdomen so it can stretch as a child grows. On occasion, the shunt may need correction or replacement.
Latex Allergy This is an extremely dangerous allergy to substances that contain latex. It is common in individuals with spina bifida. Latex allergy is a result of repeated exposure to latex, particularly in exposure to the mucous membranes. Some will develop a rash when latex touches their bodies, but many can develop severe breathing issues from inhaling latex dust and odor. Avoidance of latex products to reduce exposure is necessary. This includes many medical supplies and equipment (most are labeled as non-latex due to this severe allergy in many individuals), baby supplies like bottles, nipples and pacifiers, toys, latex balloons, and foods such as avocados, bananas, chestnuts, kiwi and passion fruit. Because latex allergy is so dangerous, parents and pediatric hospitals only allow mylar balloons.
Lymphedema A swelling in the arms or legs can be a result of slow function of the lymph system. This can occur especially in the lower extremities with spina bifida. It can appear in childhood but is more typical in adults with spina bifida. Devices are used to help the body improve lymph flow.
Obesity Individuals with chronic conditions, especially those that affect mobility, can become overweight. For those with spina bifida that affects mobility or cognition, overeating can occur. Regular consultation with a dietician can help assess the caloric need of an individual and set a healthy balanced diet to help regulate weight.
Pressure Injury For individuals with spina bifida with decreased sensation, skin care should be monitored. Pressure releases to allow blood flow, pressure dispersing equipment for sitting and in bed should be used to avoid pressure injury. Infants and babies are naturally wiggly. Infants with spina bifida may not be so wiggly. Turning, positioning and pressure dispersing equipment should be used from birth forward, even as adults.
Decreased sensation can lead to injury to the skin. Pressure injury can be from friction which separates the top layer of skin from the underlayer, shearing which is a combination of pressure and friction and pressure over pointy bony areas. The first sign of pressure injury is a discoloration of the skin. Taking measures to stay off the area until the discoloration resolves is the primary treatment. Prevention by use of pressure releases, positioning, and pressure dispersing equipment is needed.
Relating to Others Successful interactions with other children and adults is a developmental task for all individuals. All people have differing personalities being friendly, shy or other attributes. With chronic issues, children can become fearful of adults thinking a treatment is about to be delivered or overly friendly with adults due to their interactions as they are used to the adult world of healthcare. Some individuals with spina bifida have issues finding the right balance of relationships with other children or adults. Establishing opportunities and boundaries may be necessary for successful integration for you or your child.
Scoliosis As children grow, muscles in the back can develop at different rates. Some muscle groups may be stronger than other muscle groups which will cause the vertebra (back bone or spine) to pull to one side or curve in or out. Exercises for strengthening the weaker back muscles can correct milder scoliosis issues. Surgical repair to straighten the spine is also done in advanced cases.
Sleep Apnea Some individuals have breathing patterns that slow or even stop for short periods of time especially when sleeping. With spina bifida, this can occur in childhood or it might not develop until adulthood. A sleep study can identify the type of sleep apnea. Treatment with noninvasive mechanical breathing devices can improve sleep apnea. There are a variety of different facial fittings that are child and adult friendly.
Sexual Function and Infertility As adults with spina bifida, sexual function which is innervated by the last segments of the spinal cord, can be affected. Treatments to improve sexual functioning are available. For women, use of fertility treatments can generally induce pregnancy. Women with spina bifida can carry a fetus to term. Delivery can be vaginal or by cesarean section however if there is decreased or no sensation, the delivery should include all the treatments received by a woman without spina bifida as the body will still react. For men, there are a variety of mechanical and pharmaceutical treatments to achieve erection. Birth control by men and women with spina bifida must be used to prevent pregnancy.
Tethered Spinal Cord Usually, the end of the spinal cord freely floats within the spinal canal. With spina bifida, the spinal cord can be stuck to the spinal canal which then pulls or stretches the spinal cord affecting function. The spinal cord tethering is surgically released by a neurosurgeon.
Vision Some children develop strabismus or wandering eye due to an imbalance of muscles that move the eye. This is more common in children with spina bifida especially with hydrocephalus. In seeing, the eyes line up to create one image in the brain. In strabismus, the eyes do not align resulting in double vision. Eventually, the weaker eye will stop sending visual messages. In some cases, an eye patch will be used on the stronger eye to allow the weaker eye to strengthen. Eye exercises may also help strengthen the alignment. In advanced cases, surgical correction to the eye muscles is performed. In infants to one year, the eyes may appear to be misaligned as a result of developing facial structure. This is called pseudostrabismus in which vision is normal. The ophthalmologist can assist with differentiation between strabismus and pseudostrabismus.
Weakness or Paralysis In meningocele and myelomeningocele, there can be occurrence of weakness or paralysis in the lower body, decreased sensation, effects on bowel and bladder function (neurogenic bowel, neurogenic bladder) and sexual dysfunction. In myelomeningocele, trauma to the spinal cord has occurred because the spinal cord is outside of the spinal canal. Function will depend on the level and severity of the injury and the location of the neural tube injury. Mobility will be adapted for the needs of the child.
Diagnosing Spina Bifida
During Pregnancy
AFP (alpha-fetoprotein) is a routine blood test of the mother’s blood studied at 15 weeks of pregnancy. High results can indicate issues with the neural tube. The results of the AFP blood test will lead the healthcare professional to investigate further for spina bifida.
Ultrasound is a test where soundwaves are projected into the uterus that creates a picture of the fetus. Meningocele or myelomeningocele may be seen.
Amniocentesis is a test of amniotic fluid (the fluid that the fetus floats in). A needle is inserted into the mother’s abdomen to draw off a small amount of amniotic fluid. A high amount of AFP indicates spina bifida.
At Birth or Later
When the baby is born and has its first physical examination, a dimple over the spine or a tuft of hair may be the only sign of spina bifida occulta. In some cases, meningocele or myelomeningocele that was not diagnosed before birth, the pouch over the spine will be seen.
Ultrasound, MRI or CT scan is performed in the area of the dimple, hair or pouch to assess the type of spina bifida. Undiagnosed cases before birth sometimes occur if the spine area was not clearly seen on ultrasound before birth.
In adulthood Because the effects of spina bifida might not be noticed until adulthood, the diagnosis can be made later in life. Symptoms might include weakness especially in the lower extremities, urinary or bowel issues or sexual dysfunction. Diagnosis is typically made by MRI or CT scan. Although ultrasound is the typical diagnostic tool, it may not be used because spina bifida may be found in adults when looking for other neurological diagnoses.
Treating Spina Bifida
Intrauterine Surgery is sometimes performed in cases of meningocele and myelomeningocele. The mother is anesthetized, the uterus is opened, and the opening of the fetus’s spinal cord is closed. The fetus is not disconnected from the mother but still receives oxygen, nutrition and anesthesia via the umbilical cord. The baby is returned to the uterus which is re-closed until birth. The baby may be able to be born vaginally but most likely by cesarean section depending on the case. You may need to travel to a specialty center to have this unique type of surgery performed by a specialist.
If the spina bifida is not discovered until after the birth of the baby, an ultrasound, MRI or CT scan will be performed to understand the type of spina bifida. In the case of meningocele, surgery will be performed to close the opening in the spinal column and to remove the pouch. If myelomeningocele is present, surgery is done to return the spinal cord to the spinal canal along with spinal column closure and pouch removal.
Urodynamic Testing An assessment of the bladder may be indicated to understand the function of the urinary system. In a urodynamic test, a temporary catheter with sensors is placed in the bladder while fluid is flowing through an IV. A fluoroscope (light X-ray) is used to visualize the flow of urine from the kidneys, through the ureters to the bladder and out of the body while the sensors in the catheter measure pressures in the bladder and abdomen. This procedure will be done as a baseline of function typically with yearly follow up studies to monitor and correct changes.
Therapeutic treatment for success in activities of daily living (ADLs) are provided that will help the child meet developmental milestones and prepare for life. Depending on the type of spina bifida and the level of the injury, mobility, sensation and toileting can be affected. If the child has additional diagnoses, cognitive therapy should be provided.
Transitioning Care
Most incidences of spina bifida are discovered during fetal development, a few at birth and an even smaller number in adulthood. Because of early diagnosis, children grow up in a world surrounded by healthcare professionals. It can be easy for you and others to assist your child more than you might for a child without spina bifida.
Care for individuals with spina bifida is ongoing because children have changing needs as they develop. It can be difficult to transition from pediatric care to adult care where more responsibility is expected of the individual. To aid in transition, it is important for the child to know about their care needs from the onset. Use age appropriate descriptions. Milestone information can help you transition through development, transferring care and responsibility to your child. Not every milestone will match your child, but the milestone activity can be adapted to their capabilities. The earlier the child is appropriately involved in their care, the more responsible they can become for themselves especially as they transition into adulthood.
Some individuals with spina bifida occulta will not know they have the condition. Late in life, adults can notice some changes in their function due to hidden spina bifida that is now apparent due to aging. Adults who require surgery later in life might find themselves at the pediatric neurosurgeon who is familiar with closure surgeries. These are adult individuals with a pediatric issue.
Rehabilitation
Professionals involved in your child’s care include:
Pediatrician A medical professional who cares for the general health and welfare of the child. The pediatrician might be the healthcare professional that coordinates your child’s care.
Pediatric physiatrist A doctor who specializes in physical and rehabilitation medicine with an emphasis in pediatrics is a pediatric physiatrist. This person will coordinate the specific aspects of needs for improved activities of daily living, therapy and continence.
Spina Bifida Care Coordinator If care is being received at a Spina Bifida Center, there will be a person you can contact for issues through this pediatric service. If not at a Spina Bifida Center, there may be another care coordinator assigned or you will work through your pediatrician. The Spina Bifida Care Coordinator assists with organizing services, treatments and therapies through the lifespan from birth to age 21. This person will assist with hospitalization, school and home concerns for the best outcomes for your child.
Neurosurgeon A specialist in central nervous system surgery. Typically, for individuals with spina bifida, this person specializes in pediatric ages. Closure of the injury will be performed by the neurosurgeon as well as issues such as shunt placement or tethered cord release.
Urologist A medical specialist that concentrates on urinary tract function is a urologist. This specialist will follow your child through growth and development to ensure healthy renal function and effective bladder emptying.
Orthopedist A doctor who works with skeletal or bone issues. This individual may direct therapies or provide surgery for contractures(muscle, tendon, or scar tissue shortening), scoliosis or other bone-related issues.
Physical Therapist (PT) The person who will assist with gross motor movement is the physical therapist. This professional will provide therapy for mobility either by wheelchair, walking with assistive devices or ambulation. They also provide strengthening, transfers and exercises to improve health and function.
Occupational Therapist (OT) A specialist in fine motor movement and Activities of Daily Living (ADLs) is the OT. A broad range of therapies from strengthening and transfers to feeding, dressing and eating is emphasized.
Childlife Specialist The Childlife Specialist is typically found in pediatric offices and pediatric hospitals. With education in the developmental stages of children, this professional will create an environment for the best outcomes and least trauma for your child with healthcare needs.
Registered Nurse A registered nurse provides the nursing care to support and obtain best healthcare outcomes. The RN is a good resource for education as well as providing direct care.
Dietician Individuals with chronic healthcare needs often require direction for nutritious diets. Intake of calories can become an issue with mobility concerns. An assessment of age and size will direct the caloric intake balanced by energy expenditure.
Neuropsychologist A specially educated psychologist uses assessment techniques to pinpoint areas of concern in cognition, thinking and learning abilities. Once the assessment is complete, they are essential in providing strategies to create situations for best learning and outcomes.
Psychologist/Counselor Individuals and families who have members with chronic health conditions may seek direction for personal or family dynamics. The psychologist or counselor can help create strategies that are effective for each individual or family.
Teacher All school personnel involved with your child should be aware of physical and learning needs that are unique to your child as well as strategies to create the best learning environment.
Clinical Guidelines
Spina Bifida Association. Guidelines for the Care of People with Spina Bifida. 2018. https://www.spinabifidaassociation.org/guidelines/ These guidelines are for individuals across the lifespan.
The Spina Bifida Association established a Registry at the National Center for Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/ncbddd/spinabifida/nsbprregistry.html
Military Benefit
Individuals born with spina bifida, only with neurological deficit, whose parents served in the U.S. active military in wartime in Korea or Vietnam are eligible for benefits. It is thought spina bifida might be connected to Agent Orange. Benefits include lifetime healthcare, pharmaceuticals, a monthly allowance, vocational training and rehabilitation services. More information can be found on the Veterans Administration website: https://www.va.gov/COMMUNITYCARE/programs/dependents/spinabifida/index.asp
Research
A variety of research occurs regarding spina bifida. The Spina Bifida Association established a Registry at the National Center for Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/ncbddd/spinabifida/nsbprregistry.html This registry works to create a research agenda to create and coordinate research of spina bifida in a cohesive and coordinated manner.
Research of early detection, prevention and in utero surgery continue to be studied. Diagnosing, vitamin treatment prior to and during pregnancy and surgery to close the spinal opening before birth have all been developed due to extensive research. Inter-utero surgery at 19 to 25 weeks of pregnancy has been determined to greatly reduce additional injury such as hydrocephalus, brain herniation and increased ability to walk. A genetic link is being researched although there does not appear to be a family pattern. These areas continue to be refined by further research.
Many of the associated diagnoses are being studied in a variety of disciplines. There is extensive research about nutrition, learning abilities, vision and spinal cord injury along with the secondary complications of spinal cord injury. Disciplines work together to merge information across diagnostic groups to expand research.
Facts and Figures
An estimated 1,427 babies are born each year with spina bifida. Rates by ethnicity include:
- Hispanic: 3.80 per 10,000 live births
- Caucasian: 3.09 per 10,000 live births
- African American: 2.73 per 10,000 live births
Estimated cost of care for a person with spina bifida, with caregiving costs, is estimated at $791,900.
In the first year of life, hospital costs range from $21,900 to $1,350,700.
Approximately 18% of babies with spinal bifida have greater than three hospitalizations in their first year of life.
If a mother gives birth to a child with spina bifida, the risk of other children with the same issue is increased by 3%. If more than one child has spina bifida, the risks of other children with the same issue is even higher. This suggests a possibility that there could be a family link or genetic issue that has not been discovered.
Source: Centers for Disease Control and Prevention: https://www.cdc.gov/ncbddd/spinabifida/index.html
Consumer Resources
If you are looking for more information about spina bifida or have a specific question, our Information Specialists are available business weekdays, Monday through Friday, toll-free at 800-539-7309 from 9:00 am to 8:00 pm ET.
Additionally, the Reeve Foundation maintains a fact sheet about spina bifida with additional resources from trusted Reeve Foundation sources. Check out our repository of fact sheets on hundreds of topics ranging from state resources to secondary complications of paralysis.
We encourage you to reach out to spina bifida support groups and organizations, including:
Spina Bifida Association https://www.spinabifidaassociation.org/
There may be local affiliated chapters in your state, city or area.
Further Resources
References
Bowman RM, McLone DG. Neurosurgical management of spina bifida: Research issues. Special Issue: Spina Bifida – A Multidisciplinary Perspective. 2010, Volume16, Issue1, 82-87. https://doi.org/10.1002/ddrr.100
Brei T, Houtrow A. Spina Bifida. J Pediatr Rehabil Med. 2017 Dec 11;10(3-4):165-166. doi: 10.3233/PRM-170469. PMID: 29154296.
Bruner JP, Tulipan N. Tell the truth about spina bifida. Ultrasound Obstet Gynecol. 2004 Nov;24(6):595-6. doi: 10.1002/uog.1742. PMID: 15517534.
Choi EK, Kim SW, Ji Y, Lim SW, Han SW. Sexual function and qualify of life in women with spina bifida: Are the women with spina bifida satisfied with their sexual activity? Neurourol Urodyn. 2018 Jun;37(5):1785-1793. doi: 10.1002/nau.23525. Epub 2018 Mar 9. PMID: 29521435.
Donnan J, Walsh S, Sikora L, Morrissey A, Collins K, MacDonald D. A systematic review of the risks factors associated with the onset and natural progression of spina bifida. Neurotoxicology. 2017 Jul;61:20-31. doi: 10.1016/j.neuro.2016.03.008. Epub 2016 Mar 19. PMID: 27000518.
Fletcher JM, Brei TJ. Introduction: Spina bifida–a multidisciplinary perspective. Dev Disabil Res Rev. 2010;16(1):1-5. doi:10.1002/ddrr.101
Garg A, Revankar AV. Spina bifida and dental care: key clinical issues. J Calif Dent Assoc. 2012 Nov;40(11):861-5, 868-9. PMID: 23270130.
Holmbeck GN, Devine KA. Psychosocial and family functioning in spina bifida. 2010. Special Issue: Spina Bifida-A Multidisciplinary Perspective, Volume 16, Issue 1, Pages 40-46. https://onlinelibrary.wiley.com/doi/epdf/10.1002/ddrr.90
Houtrow AJ, Thom EA, Fletcher JM, Burrows PK, Adzick NS, Thomas NH, Brock JW, Cooper T, Lee H, Bilaniuk L, Glenn OA, Pruthi S, M

